Summary
Definition
History and exam
Key diagnostic factors
- presence of risk factors
- history of mechanical trauma
- past medical history of osteoporosis or neoplasm
- back pain
- bruising
- acute numbness/paraesthesia
- weakness
- muscle spasticity/clonus (hypertonicity) or hypotonia
- hyperreflexia or hyporeflexia
- Hoffman's sign
- positive Babinski's sign
- spinal deformity
- loss of anal sphincter reflex
Other diagnostic factors
- absence of bulbocavernosus reflex (S3-S4)
- signs of spinal shock (hypotonia or flaccidity that resolves within 24 hours)
- urinary incontinence
- painless urinary retention
Risk factors
- falling from a height
- high-energy mechanism of injury
- age >65 years
- concomitant osteoporosis
- previous vertebral fracture
- underlying neoplastic lesion
- underlying metabolic or inflammatory disorders
Diagnostic investigations
Investigations to consider
- thoracolumbar spine x-ray (anterior-posterior and lateral views)
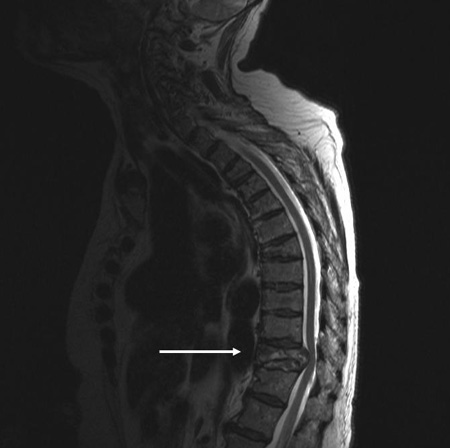
- MRI spine
- CT myelography
- MRI with STIR sequence
- Whole body CT
Treatment algorithm
Contributors
Authors
Besnik Nurboja, BSc, MBBS, MD (Res), MRCS, FRCEM
Consultant in Emergency Medicine
Emergency Medicine
Epsom and St Helier University Hospital NHS Trust
London
UK
Disclosures
BN declares that he has no competing interests.
David Choi, FRCS(SN)

Consultant Neurosurgeon and Spinal Surgeon
The National Hospital for Neurology and Neurosurgery
London
UK
Disclosures
DC declares that he has no competing interests.
Peer reviewers
Byron F. Stephens, MD, MSCI
Associate Professor
Vanderbilt University School of Medicine
Nashville
TN
Disclosures
BFS has received Institutional Research Support from Nuvasive and Stryker.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Wendt K, Nau C, Jug M, et al. ESTES recommendation on thoracolumbar spine fractures: January 2023. Eur J Trauma Emerg Surg. 2024 Aug;50(4):1261-75.Full text
American College of Surgeons. Best practices guidelines. Spine injury. Mar 2022 [internet publication].Full text
American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].Full text
National Institute for Health and Care Excellence. Spinal injury: assessment and initial management. Feb 2016 [internet publication].Full text
O'Toole JE, Kaiser MG, Anderson PA, et al. Congress of Neurological Surgeons systematic review and evidence-based guidelines on the evaluation and treatment of patients with thoracolumbar spine trauma: executive summary. Neurosurgery. 2019 Jan 1;84(1):2-6.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available here.
Use of this content is subject to our disclaimer