Summary
Definition
History and exam
Key diagnostic factors
- presence of risk factors
- abdominal pain or tenderness
- signs of ascites
- fever
- nausea/vomiting
- diarrhoea
- altered mental status
- gastrointestinal bleed
Risk factors
- decompensated hepatic state (usually cirrhosis)
- low ascitic protein/complement
- gastrointestinal bleeding
- endoscopic sclerotherapy for oesophageal varices
- ascites due to malignancy, renal insufficiency, or congestive heart failure
- extra-intestinal infection
- invasive procedures
- use of proton-pump inhibitors (PPIs)
Diagnostic investigations
1st investigations to order
- FBC
- serum creatinine
- LFT
- prothrombin time/INR
- blood cultures
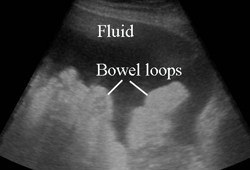
- ascitic fluid appearance
- ascitic fluid absolute neutrophil count (ANC)
- ascitic fluid culture
- ascitic fluid protein, glucose, lactate dehydrogenase (LDH), pH
Investigations to consider
- serum-ascites albumin gradient (SAAG)
- ascitic fluid carcinoembryonic antigen (CEA)
- ascitic fluid alkaline phosphatase
- ascitic fluid AFB stain and culture, fungal culture, microscopy for ova/parasites
- ascitic fluid lactoferrin
- CT scan abdomen
Emerging tests
- highly-sensitive leukocyte esterase reagent strip testing of ascitic fluid (Periscreen)
- bedside (standard urine) leukocyte esterase reagent strip testing of ascitic fluid
Treatment algorithm
Contributors
Authors
Brian Chinnock, MD
Associate Professor of Emergency Medicine
UCSF Fresno Medical Education Program
Fresno
CA
Disclosures
BC is an author of references cited in this topic.
Peer reviewers
Ke-Qin Hu, MD
Director, Hepatology Services, H.H. Chao Comprehensive Digestive Disease Center
Professor of Medicine
School of Medicine
University of California, Irvine
Irvine
CA
Disclosures
KQH declares that he has no competing interests.
Andrea De Gottardi, MD, PhD
Visiting Hepatologist
Hepatic Hemodynamic Laboratory
Liver Unit
Hospital Clinic
Barcelona
Spain
Disclosures
ADG declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Biggins SW, Angeli P, Garcia-Tsao G, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2021 Aug;74(2):1014-48.Full text Abstract
European Association for the Study of the Liver. EASL clinical practice guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018 Aug;69(2):406-60.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available here.
Guidelines
- Guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2024 update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM)
- Use of albumin infusion for cirrhosis-related complications: an international position statement
Videos
Abdominal paracentesis animated demonstration
More videos
Use of this content is subject to our disclaimer