Approach
Clinical history and examination are the basis for determining which aetiological group the pustular rash belongs to. Diagnostic tests may also help differentiate the numerous causes of a pustular rash. For example, a positive bacterial, viral, or fungal culture would point to an infectious aetiology. Eosinophils present in a skin biopsy might indicate a drug reaction.
History
History helps differentiate between the various aetiologies causing pustular eruptions. Important components of the history include:
Time of onset and duration of rash
Onset within minutes
Fire ant bites result in immediate severe burning and itching at the sting sites. Localised hive develops at the sting site within 20 minutes, followed by a necrotic lesion, termed the sterile pustule, which lasts for several days.[37]
Onset within hours
In generalised pustular psoriasis (von Zumbusch type) there is a sudden eruption (within a few hours) of generalised sterile pustules.
Onset within days
Infantile scabies should be suspected in infants or children with generalised pruritus of recent onset.
Erythema toxicum neonatorum starts soon after birth and disappears spontaneously within a few weeks without sequelae.[35]
Congenital candidiasis is acquired in utero and presents at birth or within the first few days of life. In neonatal candidiasis, mucocutaneous Candida infection, acquired during or after delivery, develops after the first few days of life.[73]
Acute generalised exanthematous pustulosis (AGEP) may occur as a sudden eruption soon after, or within 1 to 2 weeks of, exposure to certain medications; rash lasting 6 to 31 days followed by desquamation.[74][75]
Onset within weeks
Drug rash with eosinophilia and systemic symptoms (DRESS) starts within 8 weeks after initiation of therapy.[52]
Corticosteroid-induced rosacea-like eruption/corticosteroid acne occurs weeks or months after initiation of corticosteroid therapy.[76]
In syphilis, secondary-stage lesions generally appear 2 to 12 weeks after initial appearance of primary lesions.[6]
In amicrobial pustulosis of the folds (APF), relapsing pustular lesions frequently have a chronic course with recalcitrant relapses. There is usually no relation between course of the cutaneous lesions and activity of associated autoimmune disorder.[46][77]
Neonatal cephalic pustulosis (neonatal acne) may be present at birth, but more frequently appears at 2 to 3 weeks of age and resolves spontaneously.
Systemic findings or constitutional changes associated with the onset or prior to the rash
In primary infection, HSV-1 mainly causes painful gingivostomatitis.[70]
Malaise, sore throat, headache, weight loss, low-grade fever, pruritus, and muscle aches may occur with secondary syphilis.[6]
In generalised pustular psoriasis (von Zumbusch type) pustules usually erupt in waves with recurrent bouts of fever, arthralgias, and myalgias.[56]
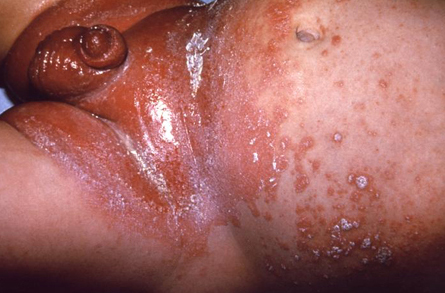
Behcet's disease is characterised by oral aphthae and by at least 2 of the following: 1) genital aphthae, 2) synovitis, 3) posterior uveitis, 4) cutaneous pustular vasculitis, 5) meningoencephalitis, 6) recurrent genital ulcers, 7) uveitis in the absence of inflammatory bowel disease or collagen vascular disease.[28][Figure caption and citation for the preceding image starts]: Mouth and genital ulcers in Behcet's diseaseFrom the collection of Dr Yusuf Yazici; used with permission [Citation ends].

Reactive arthritis classically includes the triad of conjunctivitis, urethritis, and arthritis in young male patients after gastrointestinal or urogenital infection; patients with reactive arthritis also manifest mucocutaneous symptoms: keratoderma blennorrhagicum, circinate balanitis, ulcerative vulvitis, nail changes, and oral lesions.[43]
In acne vulgaris, irregular menses, increased weight, diabetes mellitus, and/or hirsutism may point to androgen excess, resulting in acne lesions; congenital adrenal hyperplasia, polycystic ovary syndrome (PCOS), and other endocrine disorders with excess androgens may trigger development of acne vulgaris.[78][Figure caption and citation for the preceding image starts]: Nodulocystic acneUniversity of Michigan Department of Dermatology [Citation ends].

In mpox, fever, lymphadenopathy, headache, backache, and myalgia may appear before or after the rash, or not at all.[79][80][81]
Drug history
Enquire about any new medications or treatment around the time that the rash began and response to any medications used to treat the rash.
Pityrosporum folliculitis incidence can be associated with either immunosuppressive or chemotherapy treatment.[82]
Pustular drug rash secondary to epidermal growth factor receptor (EGFR) inhibitors (cetuximab, erlotinib, gefitinib) may appear between 1 to 3 weeks after onset of EGFR inhibitor treatment for colorectal or non-small cell lung cancer.[49]
Acute generalised exanthematous pustulosis (AGEP) may occur, often in female patients, after exposure to antimicrobials (commonly aminopenicillins and macrolides), diltiazem, sulphonamides, terbinafine, quinolones, paracetamol (acetaminophen), progesterone preparations, or mercury.[74][75]
In generalised pustular psoriasis (von Zumbusch type) there may be a history of drug administration with coal tar, iodides, and minocycline, or corticosteroid withdrawal.[56]
In candidal infection and disseminated candidiasis, risk factors include treatment with broad-spectrum antibiotics and corticosteroid treatment.[17][Figure caption and citation for the preceding image starts]: Infant presenting with rash formerly known as moniliasis, now called candidiasis, caused by Candida sppPublic Health Image Library, CDC [Citation ends].
In peri-oral dermatitis, over-hydration of skin caused by frequent use of occlusive moisturising emollients leads to irritation and impairment of skin barrier function; abuse of topical corticosteroids can be another triggering factor in some cases.[83]
DRESS starts within 8 weeks after initiation of therapy.[52] Medication history may include carbamazepine, phenytoin, phenobarbital, zonisamide, mexiletine, dapsone, sulfasalazine and allopurinol, sulphonamides, allopurinol, gold salts, dapsone and minocycline.
Gram-negative folliculitis should be considered in acne patients without significant improvement of acne lesions after 3 to 6 months of treatment with oral tetracyclines.[5]
Folliculitis is a rare manifestation of herpes virus infection, and should be considered in patients with folliculitis refractory to antibiotic or antifungal treatment.[84]
Past medical history
Psoriasis may be associated with pustular psoriasis.[61]
Inflammatory bowel disease may be associated with pyoderma gangrenosum.
Immunosuppression can be associated with eosinophilic folliculitis (Ofuji's syndrome/disease), folliculitis caused by herpes virus candidal infection, and disseminated candidiasis.[85]
In generalised pustular psoriasis (von Zumbusch type) there may be a history of impetigo herpetiformis in prior pregnancy or a history of trigger factors such as infections (e.g., upper respiratory tract infections), pregnancy, hypocalcaemia, and hypoparathyroidism.[56]
In pustulosis palmaris et plantaris (PPP), focal infection, such as tooth infection or tonsillitis, is a well-known exacerbating factor.[86]
APF occurs typically in association with an autoimmune or connective tissue disease, including systemic lupus erythematosus, scleroderma overlap syndrome, discoid lupus erythematosus, sicca syndrome, coeliac disease, idiopathic thrombocytopenia, or myasthenia gravis.[46][77]
Sub-corneal pustular dermatosis (Sneddon-Wilkinson disease), eosinophilic folliculitis (Ofuji's syndrome/disease), infantile acropustulosis (IA), acrodermatitis continua, PPP, Behcet's disease, and APF are recurrent conditions.
Family members with similar signs and symptoms or any sick contacts
In infantile scabies history of itching in other family members should be sought and may help diagnosis.[21][Figure caption and citation for the preceding image starts]: Scabies: characteristic linear burrows in skinFrom the collection of Dr Laura Ferris; used with permission [Citation ends].

In generalised pustular psoriasis (von Zumbusch type) there may be a family history of psoriasis.
Occupational history (e.g., contact with animals or fomites)
In cases of dermatophytosis tinea barbae, farm workers are most often affected because the usual cause is a zoophilic organism.[87][Figure caption and citation for the preceding image starts]: Tinea barbae. Note the pustules in the follicles, redness, and scalingDepartment of Dermatology Medical University of South Carolina; used with permission [Citation ends].

In orf, there may be a history of contact with lesions on animals (usually sheep or goats) or contaminated fomites.[10]
Environmental exposure
History of exposure to contaminated water in hot tubs, swimming pools, saunas, and hydrotherapy pools that are underchlorinated may suggest folliculitis caused by Pseudomonas.[88]
Pityrosporum folliculitis is more prevalent in hot and humid climates.[82]
Miliaria rubra ('prickly heat') presents in over-heated and febrile infants[38] and less commonly in adults.[40][Figure caption and citation for the preceding image starts]: Miliaria rubraFrom the collection of Brian L. Swick; used with permission [Citation ends].

Herpes simplex virus re-activation can be triggered by ultraviolet (UV) light exposure.
Clinical examination
A thorough clinical examination is essential in finding the aetiology for the pustular rash. Important considerations for the physical examination include:
Size
Folliculitis typically presents with multiple small papules and pustules on an erythematous base.[Figure caption and citation for the preceding image starts]: Superficial folliculitis with prominent erythematous papules and pustulesFrom the collection of Dr Professor Baden; used with permission [Citation ends].

In folliculitis due to Pseudomonas, 2- to 10-mm follicular papules, vesicles, and pustules, which may be crusted, are mostly seen in areas of the body that have been immersed in the contaminated water.[88]
In bullous impetigo, blisters are usually less than 3 cm in diameter.[2][Figure caption and citation for the preceding image starts]: Neonate with bullous impetigoFrom the collection of Michael Freeman; used with permission [Citation ends].

In generalised pustular psoriasis (von Zumbusch type), pustules are 2 to 3 mm in diameter usually on an erythematous base; pustules may coalesce into larger lakes of pus.
In transient neonatal pustular melanosis, superficial, 2- to 10-mm vesiculopustules without inflammation are present at or near birth.
In secondary syphilis, lesions are typically reddish brown and 3 to 10 mm in size.[Figure caption and citation for the preceding image starts]: Secondary syphilitic lesions on the facePublic Health Image Library, CDC [Citation ends].

In infantile scabies, the pathognomonic scabies burrow is an elevated white and serpiginous tract 0.3 to 0.5 mm by 10 mm long.[Figure caption and citation for the preceding image starts]: Scabies: characteristic linear burrows in skinFrom the collection of Dr Laura Ferris; used with permission [Citation ends].

In peri-oral dermatitis, erythematous papules or papulopustules are usually not larger than 2 mm.
In milia rubra, 1- to 3-mm erythematous, non-follicular-based papules and papulopustules appear due to heat.[Figure caption and citation for the preceding image starts]: Miliaria rubraFrom the collection of Brian L. Swick; used with permission [Citation ends].

In mpox, lesions are typically 5 to 10 mm in diameter.[14][79][Figure caption and citation for the preceding image starts]: Characteristic maculopapular cutaneous rashWorld Health Organization (WHO)/Brian W.J. Mahy, BSc, MA, PhD, ScD, DSc [Citation ends].
 [Figure caption and citation for the preceding image starts]: Images of individual lesions (2022 global outbreak)UKHSA [Citation ends].
[Figure caption and citation for the preceding image starts]: Images of individual lesions (2022 global outbreak)UKHSA [Citation ends].
Location and distribution
Impetigo and folliculitis caused by Staphylococcus aureus more commonly occur in areas of traumatised skin.
Folliculitis will usually occur on a hair-bearing site.[Figure caption and citation for the preceding image starts]: Superficial folliculitis with prominent erythematous papules and pustulesFrom the collection of Dr Professor Baden; used with permission [Citation ends].

Tinea barbae involves skin and coarse hairs of the beard and moustache area.[20][Figure caption and citation for the preceding image starts]: Tinea barbae. Note the pustules in the follicles, redness, and scalingDepartment of Dermatology Medical University of South Carolina; used with permission [Citation ends].

In pseudofolliculitis barbae, papules and pustules appear most commonly in the beard distribution; anterior neckline, mandibular areas, cheeks, and chin are the most common sites. There is a history of shaving or tweezing the affected area.[31]
Tinea cruris occurs in the groin area.
Tinea corporis presents on the trunk, extremities, or face.[89][Figure caption and citation for the preceding image starts]: Tinea corporis of the axilla. Central clearing with an active border of inflammation noted. Satellite lesion is presentDepartment of Dermatology Medical University of South Carolina; used with permission [Citation ends].

Tinea pedis presents with fungal maceration, and fissuring of the soles of the feet.[Figure caption and citation for the preceding image starts]: Tinea pedis. Intense inflammation produces hyperpigmentation and vesicle formation. Vesiculobullous form of tinea pedisDepartment of Dermatology Medical University of South Carolina; used with permission [Citation ends].

In acrodermatitis continua, lesions begin on 1 digit, but other digits may become involved during the chronic course of the disease.
Pustular drug rash secondary to EGFR inhibitors (cetuximab, erlotinib, gefitinib) commonly affects the face (nose, cheeks, nasolabial folds, chin, forehead), areas of the upper chest and/or back.[49]
AGEP is localised mainly to main folds (neck, axillae, groins).[74]
Transient neonatal pustular melanosis occurs predominantly on the forehead, back, posterior neck, and shins.[38]
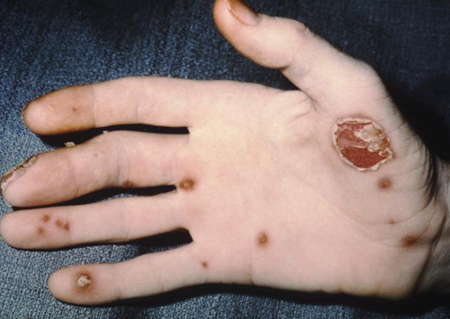
PPP is characterised by multiple pustules and erythematous plaques on palms and soles.[86]
In gram-negative folliculitis, lesions are limited to the face. Lesions consist of superficial small pustules located in the nasolabial line and on the upper lip and chin, associated with inflammatory papulopustular lesions of the cheeks and peri-oral region, or deeply sited and painful nodules of the cheeks.[90]
In secondary syphilis, painless coin-like macular lesions appear on the flank, shoulders, arms, chest, back, hands, and soles of the feet; lesions are typically reddish brown and 3 to 10 mm in size; variations of secondary syphilis skin eruptions may include pustules;[Figure caption and citation for the preceding image starts]: Secondary syphilitic lesions on the facePublic Health Image Library, CDC [Citation ends].
 other associated lesions include patchy (moth-eaten) alopecia, genital lesions (condylomata lata), superficial mucosal erosions (mucous patches).[6]
other associated lesions include patchy (moth-eaten) alopecia, genital lesions (condylomata lata), superficial mucosal erosions (mucous patches).[6]In peri-oral dermatitis, although peri-oral is the most frequent location, peri-ocular areas, nasolabial folds, and glabella may also be affected.[45]
Neonatal cephalic pustulosis (neonatal acne) is characterised by small, inflammatory, erythematous papules and pustules found on the cheeks, forehead, and scalp.[38]
In ulcerative or typical pyoderma gangrenosum, the lower extremity is the most common site of involvement.
In APF, the lesions predominate in the cutaneous folds, the scalp, the genital area, and the external auditory canal.[46]
Erosive pustular dermatosis occurs on actinically damaged scalp skin.
In mpox, the rash typically moves from the facial area distally to the extremities. In more recent outbreaks, the presentation has been atypical, with the rash presenting primarily in the anogenital region, and often not spreading further.[11][14]
Pattern of the pustules (e.g., are the pustules grouped, intact, associated with surrounding erythema, diffuse versus localised, or in a dermatomal distribution?)
In herpes simplex virus, initial lesions appear as erythematous papules that turn into grouped vesicles and pustules eventuating into crusts.[91]
In acne vulgaris, papules and pustules are associated with comedones.[Figure caption and citation for the preceding image starts]: Nodulocystic acneUniversity of Michigan Department of Dermatology [Citation ends].

In infantile scabies, classical eruption of scabies presents as pruritic papules, vesicles, pustules, and linear burrows.[Figure caption and citation for the preceding image starts]: Scabies: characteristic linear burrows in skinFrom the collection of Dr Laura Ferris; used with permission [Citation ends].

In mpox lesions may be discrete or confluent, and may be few in number or several thousand. Vesicles are well-circumscribed and located deep in the dermis. Typically, lesions simultaneously progress through four stages - macular, papular, vesicular, and pustular - before scabbing over and resolving. In atypical presentations seen in more recent outbreaks, lesions may be few and at different stages of development.[14][79]
In APF, cutaneous eruption consists of small follicular and non-follicular sterile pustules, coalescing into erosive plaques.[46]
Other clinical considerations are as follows:
Does the patient have fever?
Fever may be found in AGEP, pustular psoriasis, mpox, and cellulitis.
Are there other associated skin findings?
Erosions, ulcerations, and sinus tracts may be found in pyoderma gangrenosum.
Pitting of nails can be seen in pustular psoriasis.
Are there other systemic signs?
In generalised pustular psoriasis (von Zumbusch type), synovitis can be found in patients with related psoriatic arthritis.
Oral and genital ulcers may be present in Behcet's disease.[28][Figure caption and citation for the preceding image starts]: Mouth and genital ulcers in Behcet's diseaseFrom the collection of Dr Yusuf Yazici; used with permission [Citation ends].

Patients with reactive arthritis may have conjunctivitis and mucocutaneous symptoms: keratoderma blennorrhagicum, circinate balanitis, ulcerative vulvitis, nail changes, and oral lesions.[43][Figure caption and citation for the preceding image starts]: Pustules in a patient with reactive arthritisPublic Health Image Library, CDC [Citation ends].
Mpox may present with severe/intense anorectal pain, tenesmus, rectal bleeding, or purulent or bloody stools, associated with perianal/rectal lesions and proctitis, pruritus, dyschezia, burning, swelling, and mucus discharge. Anorectal symptoms have been unique to the 2022 global outbreak, and were not described previously.[80][81]
Diagnostic tests
Diagnostic tests are not always necessary. It is possible to make a confident clinical diagnosis of conditions such as perioral dermatitis, miliaria rubra ('prickly heat'), acne vulgaris, pustular rosacea, corticosteroid-induced rosacea-like eruption and corticosteroid acne.
Further diagnostic tests are selected depending on the likely differential diagnosis and may include microbiological tests, blood tests and skin biopsy.
Microbiological tests
Gram stain is indicated in suspected bacterial and fungal infections. It may be ordered to exclude infection in some inflammatory conditions, e.g., erythema toxicum neonatorum and neonatal cephalic pustulosis.
Skin culture for bacteria is indicated if a bacterial infection is suspected.
Potassium hydroxide (KOH) smears demonstrate hyphae and spores in fungal infection. They are indicated if a yeast or fungal infection is suspected and provide a rapid diagnosis of a fungal cause.
In candidal infection and disseminated candidiasis, serological 1,3 beta-glucan assay can be done for further confirmation.
Skin culture for fungi is indicated if a fungal or yeast infection is suspected.
Tzanck smear can be done if herpes simplex virus is suspected. Further testing for confirmation of herpes simplex virus includes direct immunofluorescence study and DNA analysis via polymerase chain reaction (PCR). Skin culture for herpes viruses may be indicated in some immunosuppressed patients.
VDRL and RPR are indicated for initial testing if clinical features of secondary syphilis are present, with further confirmation with darkfield microscopy: direct visualisation of organism, FTA-ABS test, micro-haemagglutination assay for Treponema pallidum, or histology of skin biopsy.
Microscopic mineral preparation for the presence of Sarcoptes scabieimites, eggs, or faeces (scybala) should be done if features of infantile scabies are present.
The diagnosis of mpox is confirmed by reverse-transcription PCR (RT-PCR), which would be positive for monkeypox virus or Orthopoxvirus DNA.[92]
Blood tests
Comprehensive metabolic panel and full blood count (FBC) may be abnormal if there are systemic symptoms associated with the patient's disease. These tests may be necessary prior to, or during, systemic treatment. FBC may show changes consistent with an infectious aetiology for the pustular rash.
A metabolic panel is indicated in cases of AGEP and generalised pustular psoriasis (von Zumbusch type) to evaluate for hypocalcaemia.
Erythrocyte sedimentation rate will be elevated in generalised pustular psoriasis (von Zumbusch type).
In cases of acne vulgaris, the diagnosis is usually clinical; however, further tests to evaluate the underlying cause should be considered in female patients and include free testosterone and dehydroepiandrosterone sulfate to evaluate for PCOS or an androgen-secreting tumour. LH may be elevated in PCOS. Follicle-stimulating hormone may be elevated in primary ovarian failure.
Additional testing after FBC and skin biopsy in DRESS should include liver function tests, serum creatinine level and thyroid-stimulating hormone.
Skin biopsy
Skin biopsy for routine histology and special staining should be done if the clinician narrows down the differential diagnosis, but is not absolutely sure of the diagnosis based on history and clinical examination of the patient. Special stains can help determine if the pustular rash is due to an infectious cause.
Other investigations
After skin biopsy, further testing includes serum protein electrophoresis and immunofluorescence in sub-corneal pustular dermatosis (Sneddon-Wilkinson disease).
Skin testing, enzyme-linked immunosorbent assay, or radioallergosorbent test will confirm fire ant hypersensitivity in suspected fire ant bites.
Re-challenge with the suspected drug, patch testing, interferon-gamma release assay, or in vitro testing with a macrophage migration inhibition factor test or mast cell degranulation test, are confirmatory tests for AGEP.
Plain x-ray of the involved joints, joint aspiration, and skin biopsy are indicated in reactive arthritis.
Additional testing after FBC and skin biopsy in DRESS should include urinalysis and chest x-ray.
In typical and atypical pyoderma gangrenosum, the following tests should be done to evaluate the underlying cause: hepatitis profile, serum and/or urine protein electrophoresis, peripheral blood smear, bone marrow aspiration for evidence of haematological malignancies, and investigations to exclude associated inflammatory bowel disease such as ulcerative colitis.
Use of this content is subject to our disclaimer