Aetiology
The aetiology of strabismus varies by type.
The aetiology of most infantile and paediatric forms of strabismus is poorly understood. Comitant (concomitant) strabismus seems to be a complex genetic trait, with the involvement of more than one gene. Studies suggest that genetics play an important role in childhood esotropia and exotropia.[11][12] Twin studies have revealed a concordance rate of 73% to 82% among monozygotic twins and 35% to 47% among dizygotic twins.[13] The rate for dizygotic twins is higher than the concordance for siblings, indicating that environmental factors are likely to be involved. No modifiable risk factors have been identified for most forms of comitant strabismus.
Acquired paralytic strabismus is related to malfunction of one or more of the 3 cranial nerves - oculomotor (cranial nerve III), trochlear (cranial nerve IV), and abducens (cranial nerve VI) - providing motor supply to the extraocular muscles.
Restrictive strabismus results from mechanical restriction of eye movements caused by such conditions as Graves' disease and orbital fractures.
Sensory strabismus is caused by reduced visual acuity in one eye.
Craniofacial and cranial dysinnervation syndromes and craniosynostosis may also lead to the development of strabismus.
In recurrent strabismus the abnormality recurs following initially successful treatment for the same kind of strabismus, while in consecutive strabismus the abnormality occurs following treatment for a different kind of strabismus, and residual strabismus denotes strabismus that remains after partially successful treatment.
Strabismus may also be associated with myasthenia gravis (myasthenia strabismus) and supranuclear palsies (supranuclear strabismus).
Acute-onset strabismus may be caused by an intra-cranial process such as a mass lesion, raised intra-cranial pressure, central nervous system (CNS) infarction, or inflammation in the CNS.
Strabismus is more common in children with global CNS problems, such as cerebral palsy or developmental delay.
Pathophysiology
The pathophysiology of infantile forms of strabismus (esotropia and exotropia) and intermittent exotropia is poorly understood.
Accommodative esotropia is frequently related to hyperopia (farsightedness). In hyperopia, accommodation enables a clear image to be created on the retina. Accommodation is associated with ocular convergence (eyes turning inwards); compensatory mechanisms may be overwhelmed if large amounts of accommodation are required, and esotropia can develop. Therefore, it is mandatory for all children to have a cycloplegic refraction, as this is the only way to reliably measure the refractive error in children.
Depending on the cranial nerve affected, paralytic strabismus may present with esotropia, exotropia, hypotropia, or hypertropia. The abducens nerve (cranial nerve VI) supplies the lateral rectus muscle, whose mechanism of action is to move the eye laterally. Thus, paralysis of this muscle secondary to abducens nerve palsy results in esotropia (inwards deviation of eye). The trochlear nerve (cranial nerve IV) supplies the superior oblique muscle, whose mechanism of action is to move the eye inferiorly (mainly when the eye is adducted). Thus, paralysis of this muscle secondary to trochlear nerve palsy results in hypertropia (upwards deviation of the eye). The oculomotor nerve (cranial nerve III) supplies the remaining extraocular muscles. Paralysis of these muscles secondary to oculomotor nerve palsy results in exotropia (outwards deviation of the eye due to the unopposed action of the lateral rectus muscle) and hypotropia (downwards deviation of the eye due to the unopposed action of the superior oblique muscle).
In sensory strabismus, poor vision in one eye results in disruption of fusional mechanisms designed to keep the eyes aligned. This most often leads to exotropia in older children and adults, and to esotropia in young children.
Failure of the normal innervation of the extraocular muscles in cranial dysinnervation syndromes (e.g., Duane's retraction syndrome) results in co-contraction of these muscles and subsequent abnormal deviations and movements of the eye leading to strabismus.
Strabismus is a common finding in craniofacial syndromes (e.g., Crouzon's and Apert's syndromes) and craniosynostosis, due to the abnormal orientation of the orbits in these conditions.
Classification
Direction of deviation
Horizontal
Esotropia: abnormal convergence of visual axes (inwards deviation) [Figure caption and citation for the preceding image starts]: Esotropia: left eye fixating (note decentred light reflection on right cornea)From the collection of Dr Daniel J. Salchow; used with permission [Citation ends].
Infantile esotropia: onset within first 6 months of life, usually with large and constant angle
Accommodative esotropia: onset between 18 and 24 months of age, often intermittent in the beginning, and usually associated with hyperopia (farsightedness, light focused behind the retina)
Paralytic: palsy of abducens nerve (cranial nerve VI)
Restrictive: caused by an obstacle to the free movement of the eye (e.g., Graves' disease, orbital fractures)
Sensory: secondary to poor vision in one eye
Syndromic: associated with syndromes (e.g., Duane's retraction syndrome, Brown's syndrome).
Exotropia: abnormal divergence of visual axes of the eyes (outwards deviation) [Figure caption and citation for the preceding image starts]: Exotropia: left eye fixating (note decentred light reflection in right eye)From the collection of Dr Daniel J. Salchow; used with permission [Citation ends].

Infantile: onset within first 6 months of life, less common than infantile esotropia
Idiopathic: intermittent or constant
Paralytic: palsy of oculomotor nerve (cranial nerve III), may be associated with hypotropia, ptosis, and mydriasis (pupil dilation)
Restrictive: caused by an obstacle to the free movement of the eye (e.g., orbital fractures and, less commonly than in esotropia, Graves' disease)
Sensory: secondary to poor vision in one eye.
Vertical
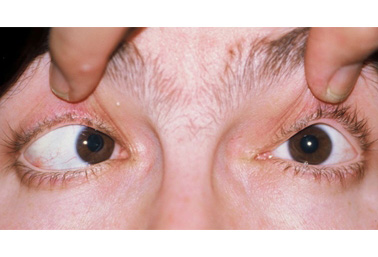
Hypertropia: upwards deviation of the visual axis of one eye relative to the other [Figure caption and citation for the preceding image starts]: Right hypertropia: left eye fixating (note inferior scleral show and decentred light reflection in right eye)From the collection of Dr Daniel J. Salchow; used with permission [Citation ends].

Paralytic: palsy of trochlear nerve (cranial nerve IV)
Restrictive: caused by an obstacle to the free movement of the eye (e.g., Graves' disease, orbital fractures).
Hypotropia: downwards deviation of the visual axis of one eye relative to the other
Paralytic: palsy of oculomotor nerve (cranial nerve III), may be associated with exotropia, ptosis, and mydriasis
Restrictive: caused by an obstacle to the free movement of the eye (e.g., Graves' disease, orbital fractures, Brown's syndrome).
Τorsional (cyclotorsion)
Incyclotorsion: eye is rotated so that the superior pole is torted nasally and the inferior pole is torted temporally, and the eye is 'rolled' towards the nose.
Excyclotorsion: eye is rotated so that the superior pole is torted temporally and the inferior pole is torted nasally, and the eye is 'rolled' towards the ear.
Frequency of deviation
Latent
No evidence of strabismus while the patient is fixating with both eyes.
Intermittent
Strabismus is present only intermittently, while at other times the eyes are aligned.
Constant/manifest
Strabismus is always present.
Variation with position of gaze
Comitant (concomitant)
Deviation does not vary in size with the direction of gaze of the fixating eye. Constitutes most forms of childhood strabismus (except those associated with cranial nerve palsy or restriction).
Incomitant (non-comitant)
Deviation varies in size with the direction of gaze of the fixating eye. Often paralytic or restrictive in nature and may indicate underlying neurological or orbital disease. If horizontal strabismus changes in size between upgaze and downgaze, the pattern is often described in analogy to letters.
A-pattern: more exotropia (or less esotropia) in downgaze compared with upgaze. Considered clinically significant if the difference is 10 prism dioptres or more.
V-pattern: more esotropia (or less exotropia) in downgaze compared with upgaze. Considered clinically significant if the difference is 15 prism dioptres or more.
X-, Y-, and lambda-pattern strabismus have also been described, but are more rare.
Fixation
Alternating
Fixation spontaneously alternates from one eye to the other.
Monocular
Definite preference exists for fixation with one eye over the other.
Age of onset
Infantile (previously known as congenital)
Strabismus documented before 6 months of age.
Acquired
Any deviation with onset after 6 months of age.
Visual function
Sensory strabismus
Associated with reduced visual acuity (poor vision) in one eye.
Underlying aetiology
Primary
Strabismus without identifiable cause. Examples include infantile esotropia and intermittent exotropia.
Secondary
Strabismus caused by an underlying disorder.
Recurrent
Strabismus that recurs following initially successful treatment for the same kind of strabismus.
Residual
Strabismus remaining after partially successful treatment.
Consecutive
Strabismus occurring after treatment for a different kind of strabismus.
Use of this content is subject to our disclaimer