Iliotibial band syndrome
- Overview
- Theory
- Diagnosis
- Management
- Follow up
- Resources
Treatment algorithm
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups: see disclaimer
pain and inflammation
non-steroidal anti-inflammatory drugs (NSAIDs)
In the acute phase, goals of treatment include reducing local inflammation and providing effective pain relief with NSAIDs.
Primary options
diclofenac potassium: 50 mg orally (immediate-release) three times daily when required
OR
ibuprofen: 400-600 mg orally every 4-6 hours when required, maximum 2400 mg/day
activity modification
Treatment recommended for ALL patients in selected patient group
Patients should be advised regarding activity modification. In mild iliotibial band syndrome (ITBS), this involves limiting physical activity up to the point (time or distance) at which symptoms begin. In severe ITBS, patients should avoid aggravating activities but can consider alternative forms of physical activity that don’t engage the affected limb. Any activity that requires repeated knee flexion and extension is prohibited. Ice should be used on the affected area.
combination local anaesthetic and corticosteroid injection
Treatment recommended for ALL patients in selected patient group
Recommended for patients with severe pain or swelling and in refractory cases.[39]Gunter P, Schwellnus MP. Local corticosteroid injection in iliotibial band friction syndrome in runners: a randomised controlled trial. Br J Sports Med. 2004 Jun;38(3):269-72. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1724827 http://www.ncbi.nlm.nih.gov/pubmed/15155424?tool=bestpractice.com
Inject in the area where the iliotibial band crosses the lateral femoral condyle.
[Figure caption and citation for the preceding image starts]: Injection site for iliotibial bandFrom the personal collection of Dr J.C. Mak [Citation ends].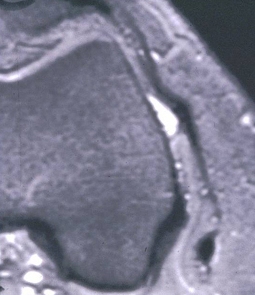
Primary options
methylprednisolone acetate: 40 mg by injection as a single dose
and
lidocaine: 10 mg by injection as a single dose
resolved pain and inflammation
stretching exercises
The subacute phase is characterised by subsiding inflammation and pain. During this phase, emphasis is on stretching of the iliotibial band and soft-tissue therapy for any myofascial restrictions (e.g., trigger points, muscle contractures, fascial adhesions) which supports muscle strengthening and re-education.[Figure caption and citation for the preceding image starts]: Standing stretch exerciseFrom the personal collection of Dr J.C. Mak [Citation ends].
foam roll mobilisation
Treatment recommended for ALL patients in selected patient group
Foam roll mobilisation can be combined with stretching exercises to improve myofascial restrictions along the lateral hip and thigh.[41]Fredericson M, Guillet M, Debenedictis L. Innovative solutions for iliotibial band syndrome. Phys Sportsmed. 2000 Feb;28(2):53-68.
http://www.ncbi.nlm.nih.gov/pubmed/20086621?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Foam roll exerciseFrom the personal collection of Dr J.C. Mak [Citation ends].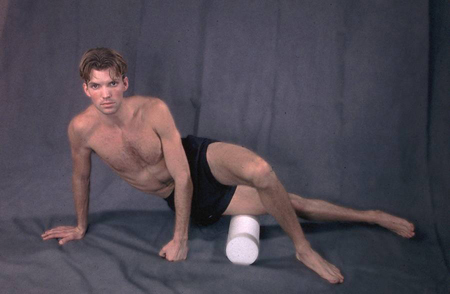
recovery and strengthening
Treatment recommended for ALL patients in selected patient group
Once range-of-motion and myofascial restrictions have been resolved with stretching exercises and foam roll mobilisation, recovery and strengthening can begin with exercises to promote movement patterns and improve hip abductor strength.
Electromyography studies suggest that contractions above 60% of the maximal voluntary isometric contraction are needed for strengthening.[42]Distefano LJ, Blackburn JT, Marshall SW, et al. Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther. 2009 Jul;39(7):532-40.
http://www.ncbi.nlm.nih.gov/pubmed/19574661?tool=bestpractice.com
[43]Ayotte NW, Stetts DM, Keenan G, et al. Electromyographical analysis of selected lower extremity muscles during 5 unilateral weight-bearing exercises. J Orthop Sports Phys Ther. 2007 Feb;37(2):48-55.
http://www.ncbi.nlm.nih.gov/pubmed/17366959?tool=bestpractice.com
This intensity is achieved with progression into single leg squat exercises and use of resistance (e.g., 2.3 kg [5 lb] ankle weight with side-lying hip abduction).[42]Distefano LJ, Blackburn JT, Marshall SW, et al. Gluteal muscle activation during common therapeutic exercises. J Orthop Sports Phys Ther. 2009 Jul;39(7):532-40.
http://www.ncbi.nlm.nih.gov/pubmed/19574661?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Demonstration of pelvic dropFrom the personal collection of Dr J.C. Mak [Citation ends].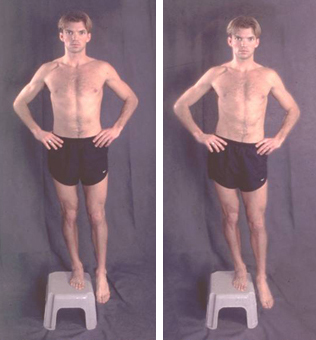
return to running
Treatment recommended for ALL patients in selected patient group
Following recovery and strengthening, patients are gradually reintroduced to running once open-chain and closed-chain exercises can be performed pain free.
refractory to conservative treatment
elective surgery
Most patients will respond to a conservative treatment approach.[38]Beals C, Flanigan D. A review of treatments for iliotibial band syndrome in the athletic population. J Sports Med (Hindawi Publ Corp). 2013;2013:367169. https://onlinelibrary.wiley.com/doi/10.1155/2013/367169 http://www.ncbi.nlm.nih.gov/pubmed/26464876?tool=bestpractice.com However, surgery may occasionally be required to decrease impingement of the ITB on the lateral femoral epicondyle. The surgery involves resection, when the leg is in a 30° flexed position, of a triangular piece of the ITB from the area overlying the lateral epicondyle. Additionally, the PLAR technique (which combines percutaneous lengthening of the ITB and arthroscopic debridement of the lateral synovial recess) may be effective in allowing a return to previous sports performance levels.[40]Arnal-Burró J, Vidal-Fernández C, Igualada-Blazquez C, et al. PLAR: a combined percutaneous and arthroscopic treatment for iliotibial band syndrome description of surgical technique and short-term results: description of surgical technique and short-term results. BMC Sports Sci Med Rehabil. 2023 Nov 10;15(1):151. https://bmcsportsscimedrehabil.biomedcentral.com/articles/10.1186/s13102-023-00723-2 http://www.ncbi.nlm.nih.gov/pubmed/37950302?tool=bestpractice.com

Choose a patient group to see our recommendations
Please note that formulations/routes and doses may differ between drug names and brands, drug formularies, or locations. Treatment recommendations are specific to patient groups. See disclaimer
Use of this content is subject to our disclaimer