Summary
Your Organisational Guidance
ebpracticenet urges you to prioritise the following organisational guidance:
Diagnose en aanpak van syfilisPublished by: KCELast published: 2020Diagnostic et prise en charge de la syphilisPublished by: KCELast published: 2020Definition
History and exam
Key diagnostic factors
- presence of risk factors
- anogenital ulcer
- lymphadenopathy
- diffuse rash
- constitutional symptoms
- fatigue
- rhinitis (congenital syphilis)
- hepatosplenomegaly (congenital syphilis)
- patchy alopecia
- condylomata lata
- memory impairment, altered mood, confusion, or dementia
- visual changes
- Argyll-Robertson pupils
- loss of sense of vibration, proprioception, and position sense
- ataxia
- loss of anal and bladder sphincter control
- positive Romberg's sign
- diastolic murmur
- rubbery lesions/nodules with a necrotic centre
- miscarriage, stillbirth, or neonatal death (congenital syphilis)
- premature labour and intrauterine growth retardation (congenital syphilis)
- neonatal skin rash (congenital syphilis)
- tibial bowing (congenital syphilis)
- craniofacial malformation (congenital syphilis)
- tooth abnormalities (congenital syphilis)
- necrotising funisitis (congenital syphilis)
Other diagnostic factors
- mouth ulcer
- asymptomatic with positive serology (latent syphilis)
- tremor
- headache
- meningismus
- eye pain
- hearing loss
- seizures
- peripheral oedema
- jaundice
- peripheral neuropathy
- areflexia
- angina
- dyspnoea
- organomegaly
- skin or visceral organ perforation or collapse of structure
- neonatal neurological abnormalities (congenital syphilis)
Risk factors
- sexual contact with an infected person
- men who have sex with men (MSM)
- illicit drug use
- commercial sex workers
- multiple sexual partners
- people with HIV or other STIs
- syphilis during pregnancy (risk for congenital syphilis)
Diagnostic investigations
1st investigations to order
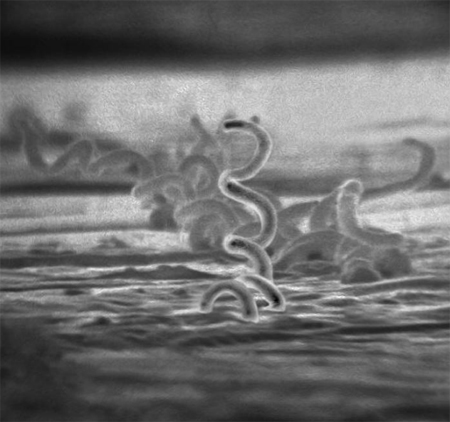
- dark-field microscopy of swab from lesion
- serum treponemal enzyme immunoassay (EIA)
- chemiluminescence immunoassay (CLIA)
- serum Treponema pallidum particle agglutination (TPPA)
- serum Treponema pallidum haemagglutination (TPHA)
- serum Treponema pallidum latex agglutination (TPLA)
- serum fluorescent treponemal antibody absorption (FTA-ABS) test
- immunocapture assay
- line immunoassay (LIA) serological test
- serum rapid plasma reagin (RPR) test
- serum Venereal Disease Research Laboratory (VDRL) test
Investigations to consider
- lumbar puncture, cerebrospinal fluid (CSF) analysis
- CXR
- echocardiogram
- CT brain
- MRI brain
- HIV test
- fetal ultrasound scan
- FBC
- long-bone x-rays
- liver function tests (aspartate aminotransferase, alanine aminotransferase and alkaline phosphatase) and bilirubin
- auditory brainstem response
- audiometry
- fetal skeletal survey
Emerging tests
- Treponema pallidum polymerase chain reaction (PCR) (sample taken directly from ulcerative lesions)
- point of care (POC) testing with either treponemal or combination treponemal/non-treponemal antibody
Treatment algorithm
Contributors
Authors
Juan C. Salazar, MD, MPH, FAAP
Professor and Chair
Department of Pediatrics
University of Connecticut School of Medicine
Physician in Chief
Connecticut Children’s
Hartford
CT
Disclosures
JCS has received NIH funding for syphilis research. JCS has been invited to speak about syphilis and congenital syphilis at various international conferences. He has been the principal author, corresponding author and/or co-author of several papers in the field of syphilis vaccine development, syphilis molecular epidemiology, and syphilis pathogenesis. JCS is the author of references cited in this topic.
Acknowledgements
Dr Juan C. Salazar would like to gratefully acknowledge Adriana R. Cruz, Jairo M. Montezuma-Rusca, Nicholas Bennett, Patrick French, and Nooshin Barmania, previous contributors to this topic. We would also like to acknowledge our infectious diseases expert panel member, Dr Elisabeth Adderson, for her contribution to this topic.
Disclosures
PF is an author of a reference cited in this topic. EA, ARC, JMMR, NB, and NB declare that they have no competing interests.
Peer reviewers
Robert A. Larsen, MD
Associate Professor of Medicine
University of Southern California
Keck School of Medicine
Los Angeles
CA
Disclosures
RAL declares that he has no competing interests.
William Rodriguez, MD
Assistant Professor of Medicine
Harvard Medical School
Director of Research
Global Health Delivery Project
Harvard School of Public Health
Boston
MA
Disclosures
WR declares that he has no competing interests.
Jennifer Handforth, MB ChB, MRCPCH, DTM&H
Consultant Paediatrician
Croydon University Hospital
Croydon
UK
Disclosures
JH declares that she has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Stoltey JE, Cohen SE. Syphilis transmission: a review of the current evidence. Sex Health. 2015 Apr;12(2):103-9.Full text Abstract
Kingston M, Apea V, Evans C, et al. BASHH UK guidelines for the management of syphilis 2024. Int J STD AIDS. 2024 Dec;35(14):1142-60.Full text Abstract
World Health Organization. Guidelines for the treatment of Treponema pallidum (syphilis). 2016 [internet publication].Full text
Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187.Full text Abstract
World Health Organization. WHO guideline on syphilis screening and treatment for pregnant women. 2017 [internet publication].Full text
Reference articles
A full list of sources referenced in this topic is available here.
Use of this content is subject to our disclaimer