Investigations
1st investigations to order
ECG
Test
Always perform an ECG in any patient with acute chest pain to rule out ST-elevation myocardial infarction.[2][6][17][31] See ST-elevation myocardial infarction.
However, be aware that myocardial ischaemia or infarction may be present in patients with aortic dissection, which can mask the diagnosis of dissection.[2] This may be due to:
Aortic false lumen expansion causing compression or obliteration of the coronary ostia
Propagation of the dissection into the coronary arteries.
Result
ST segment depression may occur with acute dissection; ST elevation occurs rarely
CT (chest, abdomen, and pelvis)
Test
Use urgent CT from neck to pelvis as first-line imaging for definitive diagnosis of aortic dissection.[2][14][31] Trans-oesophageal echocardiography and MRI are alternatives, depending on local expertise and availability and the patient’s haemodynamic status.[2][17] In practice, CT may also be used as initial imaging for suspected aortic dissection instead of transthoracic echocardiography (TTE) if this is unavailable or inconclusive, and the patient is haemodynamically stable.
A protocol of non-enhanced CT, followed by contrast-enhanced CT angiography is recommended.[2] This should include CT neck-pelvis to visualise the extent of the dissection.[2]
The European Society of Cardiology recommends that contrast CT neck-pelvis should be performed without delay and/or focused TTE and ECG if acute aortic syndrome is suspected and a patient is calculated to have an aortic dissection detection-risk score (ADD-RS) of ≥2 (high risk) using the following criteria:
High-risk condition: if one present = 1 ADD-RS point
Marfan syndrome; family history of aortic disease; known aortic valve disease; recent aortic manipulation; known aortic aneurysm
High-risk pain feature: if one present = 1 ADD-RS point
Chest, back, or abdominal pain described as abrupt onset, severe intensity, or ripping/tearing
High-risk examination feature: if one present = 1 ADD-RS point
Haemodynamic instability (hypotension/shock); perfusion deficit (pulse deficit, differential systolic blood pressure); focal neurological deficit; new aortic regurgitation murmur
[Figure caption and citation for the preceding image starts]: CT of a 71-year-old man showing type II dissecting aneurysm of the ascending aorta. Haematoma around the proximal segment of the ascending aorta (panels A-D) compressed the right pulmonary artery, almost occluding its patency and limiting the perfusion of the reciprocal lung [Citation ends].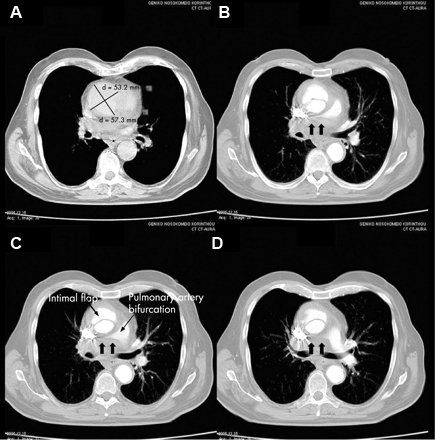 [Figure caption and citation for the preceding image starts]: CT scan showing dissecting aneurysm in a 45-year-old patient with Marfan syndrome experiencing chest pain [Citation ends].
[Figure caption and citation for the preceding image starts]: CT scan showing dissecting aneurysm in a 45-year-old patient with Marfan syndrome experiencing chest pain [Citation ends].
Result
intimal flap in acute and chronic dissection; in chronic dissection the flap may be thickened and there may be evidence of calcification and fewer periaortic reactive changes
echocardiography
Test
Although the European Society of Cardiology recommends that transthoracic echocardiography (TTE) should be used during initial investigation, in the UK, TTE may not be available in some accident and emergency departments and may give poor quality images.[17] In practice, organise CT if TTE is unavailable or inconclusive and the patient is haemodynamically stable.[2][17]
Consider trans-oesophageal echocardiography (TOE) for definitive diagnosis of acute aortic dissection in addition to TTE, depending on local expertise and availability.[2]
For type A dissections (ascending), TOE may be performed in the ICU or operating theatre to confirm the diagnosis and better evaluate the aortic valve.
Sensitivity and specificity for TOE are higher than for TTE.
CT and MRI are alternatives, depending on local availability and the patient’s haemodynamic status.[2]
TOE can also be used to confirm the diagnosis of chronic dissection.[2][Figure caption and citation for the preceding image starts]: Trans-oesophageal echocardiography (transverse aortic section) showing a circumferential dissection of the ascending aorta in a 30-year-old patient with features of Marfan's syndromeBouzas-Mosquera A, Solla-Buceta M, Fojón-Polanco S. Circumferential aortic dissection. BMJ Case Reports 2009; doi:10.1136/bcr.2007.049908 [Citation ends].
Result
intimal flap in acute or chronic dissection; two lumens may be seen in chronic dissection
CXR
Test
Order a CXR for all patients, if the clinical situation allows.[6]
If chest x-ray shows widening of the mediastinum or pleural effusion, this can indicate aortic dissection; organise further definitive imaging with CT.[14] TOE and MRI are alternatives.[2][34] However, if you have a high suspicion of aortic dissection, do not delay definitive imaging for aortic dissection, even if the chest x-ray is normal.[6]
Result
contour of the aortic knob; 'calcium sign', which appears as a separation of the intimal calcification from the aortic wall of >5 mm; tracheal deviation to the right; mediastinal widening; double density appearance within the aorta; deviation of the nasogastric tube to the right
high-sensitivity troponin
Test
Important to exclude myocardial infarction. However, be aware that myocardial ischaemia or infarction may be present in patients with aortic dissection, which can mask the diagnosis of dissection.[2] This may be due to:
Aortic false lumen expansion causing compression or obliteration of the coronary ostia
Propagation of the dissection into the coronary arteries.
Result
usually negative
renal function tests
Test
May show renal failure; either pre-existing, or developing if renal perfusion is compromised.[2]
Result
elevated creatinine and urea
liver function tests
Test
May be elevated if hepatic perfusion is compromised.
Result
elevated aspartate transaminase and alanine transaminase
lactate
Test
Indicative of bowel ischaemia or metabolic acidosis due to ischaemia caused by aortic dissection.
Result
elevated or normal
FBC
Test
Anaemia may be present in the case of haemorrhage.
May show signs of inflammation due to an inflammatory response (such as systemic inflammatory response syndrome [SIRS]) as a consequence of aortic dissection.[40]
Result
reduced or normal red blood cell count; evidence of inflammation
CRP
group and save/cross match
Test
Surgical intervention/transfusion may be necessary in some cases.
Result
preparation for surgery
blood gas
Test
Perform a blood gas in all patients.
Result
may show metabolic acidosis
creatine kinase
Test
May be elevated due to reperfusion injury or rhabdomyolysis.[2]
Result
may be elevated
coagulation studies
Test
Indicated if ruptured or symptomatic abdominal aortic aneurysm is suspected.
Result
baseline levels
Investigations to consider
D-dimer
Test
Order a D-dimer (preferably point-of-care) if you have a low clinical suspicion of aortic dissection.[2]
Despite a high sensitivity, D-dimer is not recommended as the sole screening tool for acute aortic dissection; while negative D-dimer may be helpful to rule out aortic dissection in a patient with a low clinical suspicion of dissection, a positive D-dimer lacks specificity when used in isolation.[36][37]
However, D-dimer is useful when considering the differential diagnosis (e.g., pulmonary embolism).[17][38]
When D-dimer levels are below 500 ng/mL, acute aortic dissection is unlikely.[2][39]
Result
positive
magnetic resonance angiography
Test
Magnetic resonance angiogram is the most accurate, sensitive, and specific test for aortic dissection, but is rarely used in the acute setting because it is more difficult to obtain than CT.[2][14][17] It should only be used if the patient is haemodynamically stable; CT and TOE are alternatives depending on local expertise and availability.[2][14][17]
Result
intimal flap in acute or chronic dissection; in chronic dissection the flap may be thickened and there may be evidence of calcification and fewer periaortic reactive changes; two lumens may be seen in chronic dissection
intravascular ultrasound
Use of this content is subject to our disclaimer