Investigations
1st investigations to order
ultrasound of liver
Test
An initial imaging test for high-risk patients, such as those with a high risk of cirrhosis or known cirrhosis, to screen for hepatocellular carcinoma (HCC). It is widely available and non-invasive.[64]
Patients with lesions <1 cm on initial screening ultrasound are typically monitored with a further ultrasound and alpha fetoprotein (AFP) every 3-6 months.[7] If the lesion demonstrates no growth after two or more follow-up ultrasound examinations, these patients may revert to routine surveillance (ultrasound and AFP every 6 months).[7]
The sensitivity of ultrasound for HCC detection is 60% and the specificity 97%.[65] Contrast-enhanced ultrasound may be considered as an add-on to characterise indeterminate nodules, but CT and MRI are preferred for subsequent imaging because these modalities have higher sensitivity and can analyse the whole liver.[2][62][70]
Result
poorly defined margins and coarse, irregular internal echoes
FBC
Test
Patients with low mean corpuscular volume (MCV) and low haemoglobin may have possible variceal bleeding. However, high MCV can be seen in patients with HCC due to alcohol-related cirrhosis.
Low platelet count is indicative of portal hypertension resulting from cirrhosis.
Result
microcytic anaemia and/or thrombocytopenia
basic metabolic panel
Test
Patients may have hyponatraemia due to volume overload or diuretic use.
Urea can be elevated secondary to prerenal azotaemia, acute renal insufficiency, chronic renal insufficiency, or hepatorenal syndrome.
Result
hyponatraemia; high urea
liver function tests
Test
Can be used initially to measure the severity of liver disease.
Transaminases, alkaline phosphatase, and bilirubin are elevated in conjunction with low albumin due to chronic liver disease and cirrhosis.
Good liver functional status is required for tumour resection, thereby preventing decompensation of liver or liver failure after resection.
Result
elevated aminotransferases, alkaline phosphatase, and bilirubin; low albumin
prothrombin time/INR
Test
Measures the synthetic function of the liver. It is helpful to determine the synthetic functional capacity of the liver if a patient is a candidate for liver resection or liver transplantation.
Result
normal or elevated
viral hepatitis panel
Test
Determines a viral cause (hepatitis B and C) of cirrhosis resulting in HCC.
Result
may be positive
alpha fetoprotein (AFP)
Test
Serum AFP levels can be helpful, although they are elevated in only 60% of patients with HCC (typically those with the most advanced disease), hence a normal AFP level does not rule out HCC.[66] Further, elevated AFP levels can also occur in, for example, intrahepatic cholangiocarcinoma, gastric cancer, and germ cell tumours.[7] A rise in serum AFP in a patient with cirrhosis should raise the suspicion for HCC. Mild elevations may occur in patients with chronic hepatitis without HCC. Sensitivity ranges from 41% to 65%, and specificity ranges from 80% to 94%.[67] Specificity increases with higher AFP levels.[68] AFP may be used in conjunction with abdominal ultrasound when screening for HCC.
Result
may be elevated
Investigations to consider
contrast CT scan of abdomen
Test
If there is an elevated alpha fetoprotein and/or abnormal ultrasound with focal liver lesion(s), then multiphasic CT or dynamic contrast-enhanced MRI of the abdomen should be ordered to confirm the diagnosis of hepatocellular carcinoma (HCC).[2][7][69]
The National Comprehensive Cancer Network (NCCN) suggests dynamic contrast-enhanced CT (or MRI) as an alternative to ultrasound for screening and surveillance if ultrasound is unable to detect nodules or if visualisation is poor.[2]
CT is usually more readily available than MRI, and the choice between the two modalities is typically centre-dependent.
CT scans of the abdomen have a sensitivity of 68% and a specificity of 93% in the diagnosis of HCC.[65]
Non-invasive diagnosis of HCC should be based on the Liver Imaging Reporting and Data System (LI-RADS) criteria.[2][62] ACR: Liver Imaging Reporting and Data System (LI-RADS®) Opens in new window
Result
typical hypervascular pattern
contrast MRI of abdomen
Test
If there is elevated alpha fetoprotein and/or abnormal ultrasound with focal liver lesion(s), then multiphasic CT or dynamic contrast-enhanced MRI of the abdomen should be ordered to confirm the diagnosis of hepatocellular carcinoma (HCC).[2][7][69]
The National Comprehensive Cancer Network (NCCN) suggests dynamic contrast-enhanced MRI (or CT) as an alternative to ultrasound for screening and surveillance if ultrasound is unable to detect nodules or if visualisation is poor.[2] The sensitivity of MRI of the abdomen for diagnosing HCC is 81%; specificity is 85%.[65]
MRI is superior to CT scan of the abdomen in differentiating dysplastic nodules, vascular lesions (haemangioma), and focal fat from HCC. However, one Cochrane review found that MRI may miss up to 16% of people with HCC, and 6% of patients without HCC may be treated unnecessarily.[71]
[  ]
MRI is usually less readily available than CT, and the choice between the two modalities is typically centre-dependent.
]
MRI is usually less readily available than CT, and the choice between the two modalities is typically centre-dependent.
Non-invasive diagnosis of HCC should be based on the Liver Imaging Reporting and Data System (LI-RADS) criteria.[2][62] ACR: Liver Imaging Reporting and Data System (LI-RADS®) Opens in new window
[Figure caption and citation for the preceding image starts]: MRI: hypervascularity on the arterial phaseFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: MRI: washout portal phaseFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI: washout portal phaseFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].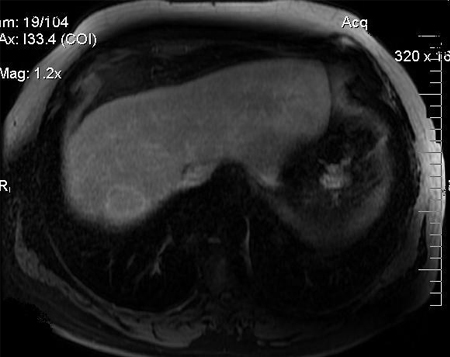 [Figure caption and citation for the preceding image starts]: MRI: following transarterial chemo-embolisation treatmentFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI: following transarterial chemo-embolisation treatmentFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].
Result
high-intensity pattern on T2-weighted images and a low-intensity pattern on T1-weighted images on MRI
liver biopsy
Test
Most of the time, the diagnosis of HCC can be made radiologically in patients with cirrhosis without the need for liver biopsy. However, biopsy should be considered if the lesion remains indeterminate and in order to establish diagnosis of HCC in patients without cirrhosis or chronic hepatitis B virus infection.[7]
An ultrasound-guided percutaneous liver biopsy is favoured.
Core needle biopsy may be considered in certain clinical scenarios.[2]
Biopsy of liver lesions may also be necessary if clinical features suggest the possibility of metastatic liver disease or cholangiocarcinoma.
[Figure caption and citation for the preceding image starts]: Medium power microscopic view of a haematoxylin and eosin stained section depicting normal liver on the right and HCC on the left. A sharp boundary separates the distinct zones of normal liver and tumourFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].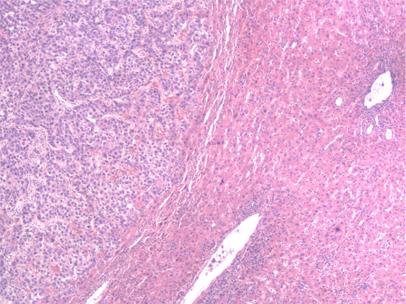 [Figure caption and citation for the preceding image starts]: High-power view of haematoxylin and eosin stained section of a well-differentiated HCC. Predominantly a solid pattern of growth with some nesting of malignant cells, separated by compressed sinusoids; some cells have clearing of the cytoplasmFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: High-power view of haematoxylin and eosin stained section of a well-differentiated HCC. Predominantly a solid pattern of growth with some nesting of malignant cells, separated by compressed sinusoids; some cells have clearing of the cytoplasmFrom the personal collection of Badar Muneer MD, Florida Hospital Transplant Center, Orlando, FL; used with permission [Citation ends].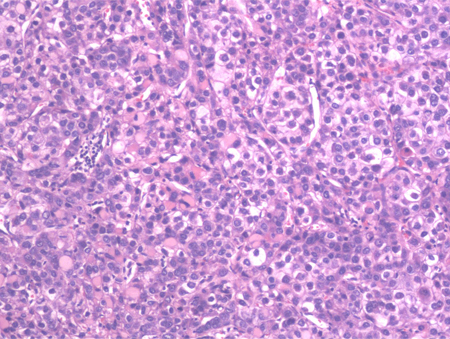
Result
well-differentiated to poorly differentiated hepatocytes with large multinucleated giant cells having central necrosis
CT scan of chest
Test
Can rule out metastatic hepatocellular carcinoma (HCC).[64]
Result
enhancing nodule or mass in the lungs is suggestive of metastatic lesion from HCC
Use of this content is subject to our disclaimer