Recommendations
Urgent
Assess the patient using the Airway, Breathing, Circulation, Disability, Exposure (ABCDE) approach.[44]
Assess the patient's pain immediately, and again within 30 minutes of administering initial analgesia.[45]
Request an orthopaedic opinion urgently.
Involve the multidisciplinary team (including orthopaedic and orthogeriatric input if the patient is older and/or frail).
Establish whether there was a fall and, if so, the cause.
Check for other injuries, including significant head injury or rib fractures.
Ensure a thorough clerking, including comorbidities (e.g., anaemia, diabetes, arrhythmia, dementia, or infections), medications, and functional status.
Order plain radiographs in all patients with a history of a fall or trauma who present with hip pain.[45]
Request further imaging if there is no obvious fracture on plain radiographs and patient has ongoing hip pain or is unable to weight bear.
Key Recommendations
Presentation
Patients typically present with hip pain following a fall or trauma, with substantially reduced movement around the joint and inability to bear weight.
A shortened and externally rotated leg may indicate a displaced fracture.[1][48]
Hip fracture can be easily missed in patients with severe cognitive impairment presenting with inability to weight bear. A multidisciplinary approach to assessment involving nursing staff, a physiotherapist, and a geriatrician may be required to reach the diagnosis.
Request an orthogeriatric assessment to support preoperative optimisation.
Analgesia
Provide immediate analgesia, even before investigations.[45]Provide analgesia to patients with cognitive impairment even if not reporting pain.[45]
Use your hospital’s prescribing protocol or National Institute for Health and Care Excellence (NICE) recommendations (see Management - recommendations section for further details).[45]
History
History is usually specific for a fall from a standing height or trauma. Consider pathological fracture if no fall.[49]
Investigations
Order a full blood count, urea and electrolytes, glucose, clotting and group and save, and ECG to assess cardiac status.[46] Consider a chest radiograph in those with a history of cardiorespiratory disease.
Imaging
Order plain radiographs with both anteroposterior pelvic and lateral views.
Radiography is the definitive test to confirm the diagnosis.[1]
Consider ordering any other radiographs needed at the same time to prevent the patient being moved twice (e.g., chest, looking for other bony injuries).
If the radiograph does not show a fracture but you strongly suspect a hip fracture (due to groin/hip/femur pain and non-weight bearing), request an MRI scan.[45]
Order a CT scan if MRI is not available within 24 hours or is contraindicated.[45] Check your local hospital protocol.
Technetium bone scan may also be used if there is no access to an MRI or CT; however, the bone scan may be falsely negative for up to 72 hours from the time of injury.[50]
Classify fractures radiographically into intracapsular and extracapsular to determine surgical management.[1]
These may be further subdivided, depending on the level of the fracture and the presence or absence of displacement and comminution.[1]
Assess mental state
Use a standardised and validated measure to check for cognitive impairment.[51][52]
Patients typically present after a fall with pain in the hip, groin, or femur; substantially reduced movement around the joint; and inability to bear weight. The leg is usually shortened and externally rotated.[1][48]
Assess the patient using the ABCDE approach, and involve the multidisciplinary team.[44]
History of fall or trauma
Ask about a recent fall or trauma. The predominant mechanism of injury is a fall.[1][48]
In older patients, falling from a standing height can cause hip fracture.
Pain in the affected hip, groin, or thigh
Global pain is typically reported around the groin and the region of the greater trochanter.[1]
May radiate distally down the femur or up to the pelvis.[53]
Pain is often increased with internal or external rotation of the leg or flexion of the hip.
Patients with severe cognitive impairment may present without obvious pain but with inability to weight bear.[54]
Inability to bear weight or move the hip
Weight bearing is either impossible or causes pain in the groin, hip, or femur.[1][48]
The leg cannot support body weight if the fracture is displaced.[53]
Straight leg raising is unlikely to be possible (although it may be possible in a patient with an undisplaced fracture).
Shortened, externally rotated leg
A shortened and externally rotated leg may indicate a displaced fracture.[1][48]
Assess and treat the patient's pain immediately and reassess 30 minutes after administering analgesia.[45]
Use a pain assessment score.
Continue to assess pain hourly until the patient is settled on the ward, and then regularly thereafter.[45]
Provide immediate analgesia, even before a diagnosis, to make investigations more comfortable for the patient (e.g., to transfer the patient from trolley to x-ray table).[45]
Use your hospital’s prescribing protocol, or NICE recommendations (see Management recommendations for further details).[45]
Provide analgesia to all patients regardless of mental state.[45]
Consider adding nerve blocks to analgesia if there is insufficient pain relief or to limit opioid dosage.[45] Opioid analgesia may exacerbate delirium and a fascia iliac block may reduce postoperative and total analgesia requirements.[55]
Take a detailed history. You should establish whether there was a fall and, if so, the cause (e.g., accidental, loss of balance, syncope, intercurrent illness).The hip fracture may be the presenting complaint of a previously undiagnosed medical issue.
Medical
Ask about:
Pain in the groin, hip, or thigh
Inability to bear weight or move the hip
Recent fall or trauma
Most fractures in older patients are from falls from a standing height.[1][48]
Assess the cause of the fall (e.g., whether this was a simple mechanical trip or a fall resulting from a medical condition). Gait and balance problems, muscle weakness, visual impairment, cognitive impairment, depression, functional decline, and particular medications are the most common underlying causes and risk factors for falls.[29][30] The causes of falls may be inter-related and multifactorial. See Assessment of falls in the elderly.
Patients with low bone mineral density, as in osteoporosis, may rarely have no history of trauma.
High-energy trauma (e.g., motor vehicle accident) is more common in younger patients.[17]
Any loss of consciousness with the injury
Previous falls or fractures
Osteoporosis or vitamin D deficiency
Osteoporosis is a strong risk factor
Low hip bone mineral density weakens the proximal femur and increases the risk of hip fracture.[27]
Cardiovascular, renal, or endocrine disorders
Mental state, especially dementia
Continence
Malignancy
Pathological fractures can be caused by metastatic cancer or, rarely, a primary bone tumour.[49]
Prodromal pain, history of malignancy, or night pain raise suspicion of metastatic bone disease and should be documented along with any circumstances of injury.[9]
Patients with breast cancer or prostate cancer may be particularly at risk due to a loss in bone mineral density after chemotherapy or hormone therapy.[56][57]
Social
Ask about:
Falls
Age
Smoking
Alcohol consumption
Ask about recent or regular alcohol consumption. It can increase the risk of falls and osteoporosis.
Usual mobility and activity levels
Ask about ability to walk indoors and outdoors (accompanied or unaccompanied).[59]
Ask about the use of walking aids (walking sticks or frame).
Ask whether the patient has stairs in their usual place of residence.
Social circumstances
Ask whether the patient lives independently or has a carer.
Medication
Consider medications that may need to be reviewed or reversed prior to surgery, such as:
Anticoagulants – increase the risk of bleeding after a fall and may need to be reversed prior to surgery.[60] Ask specifically about direct oral anticoagulants and warfarin
Oral hypoglycaemics and/or short-acting insulin
Medications that may cause perioperative hypotension, such as antihypertensives or alpha-blockers, or increase the risk of acute kidney injury, such as ACE inhibitors and angiotensin receptor blockers.
Ask about drugs that increase the risk of fracture or falls.
Drugs that increase the risk of fracture:
Levothyroxine – decreases bone density[61]
Loop diuretics – impair calcium absorption in the kidneys[62]
Corticosteroids – long-term use can lead to osteoporosis.[33] If the patient has been taking corticosteroids for a long time, they may have adrenal suppression requiring an increase of the corticosteroid dose around the time of surgery[34][63][64]
Long-term bisphosphonates – rarely associated with atypical hip fractures.[65] Identify whether a patient is already taking a bone protection medication and, if so, how long they have been taking it for.
Drugs that increase the risk of falls:
Medications that cause sedation (e.g., antidepressants, sedatives) – increase the risk of falls due to sedation[29]
Antihypertensives – may increase the risk due to adverse effects such as postural hypotension and dizziness[35]
Opioid analgesics – may increase the risk through their sedative effects.[29][66]
Family
Ask whether there is a family history of fractures or osteoporosis.
Collateral
Ask about:
The mechanism of the fall and whether there was a loss of consciousness
A relative or witness may give different answers from the patient.
The patient’s baseline level of functioning:
How does the patient usually manage at home?
How independently can they walk, get undressed, or go to the toilet?
Is there any cognitive impairment?
Always assess patients with trauma with an ABCDE approach.[44]
Check for other injuries that may have occurred as a result of the trauma (e.g., intracranial haemorrhage or facial fractures).
Assess the patient using an early warning score, such as the National Early Warning Score (NEWS2).[67] See the Risk stratification section in Management recommendations for further details.
Hip examination
Perform an examination of the hip.
Look for a shortened and externally rotated leg, which indicates a displaced fracture.[48]
Check for deformities of the limb.
Look for ecchymosis – rarely present.
Palpate for tenderness over and around the groin.
Assess (if possible without causing pain):
External rotation and abduction of the affected limb
Pain elicited with rotation of the limb
Distal pulses and sensation.
Ask the patient to perform an active straight leg raise.[68] Patients with a hip fracture are unlikely to be able to perform this manoeuvre (although it may be possible in a patient with an undisplaced fracture).
Systems examination
In addition to the hip examination, perform a thorough physical examination of the cardiac, respiratory, and neurological systems and skin.
Order plain radiographs in all patients with a history of a fall or trauma who present with hip pain.[45]
At least 90% of proximal femoral fractures will be identified on radiographs.[50][69]
Request anteroposterior (AP) pelvic radiograph and lateral views of the affected hip.
Look for a fracture of the proximal femur.
On the AP view, look for interruption of the smooth curve known as Shenton’s line (from the inferomedial border of the femoral neck to the inferior border of the superior pubic ramus), increased density of bone due to impaction at the fracture site, and any breach in the cortex either medially or laterally.
On the lateral view, look for anterior displacement of the femoral shaft/neck relative to the head, increased density of bone due to impaction, and any breach in the cortex.
Order a radiograph of the femur if you suspect distal extension of the fracture.
Consider ordering any other radiographs needed at the same time to prevent the patient being moved twice (e.g., chest, looking for other bony injuries).
If the patient has a history of malignancy, request a full-length radiograph of the femur to identify bony metastases.[70]
Order an MRI scan if you have a high clinical suspicion of hip fracture despite a negative plain radiograph (i.e., severe pain, and/or shortened and externally rotated leg).[45]
MRI has a higher sensitivity for occult hip fractures, and is not contingent on time between injury and the imaging.[71][72]
Order a CT scan of the pelvis or technetium bone scan if MRI is not immediately available or is contraindicated.[45]
A CT scan is useful for picking up alternative causes for hip pain, such as pubic rami fractures, acetabular fractures, and iliopsoas haematoma.
[Figure caption and citation for the preceding image starts]: Initial anteroposterior radiograph showing a displaced left hip intracapsular fractureFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
 [Figure caption and citation for the preceding image starts]: Unstable intertrochanteric fracture on x-rayFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
[Figure caption and citation for the preceding image starts]: Unstable intertrochanteric fracture on x-rayFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends]. [Figure caption and citation for the preceding image starts]: Magnetic resonance imaging showing coronal imaging confirming an intracapsular fracture of the left hipFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
[Figure caption and citation for the preceding image starts]: Magnetic resonance imaging showing coronal imaging confirming an intracapsular fracture of the left hipFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].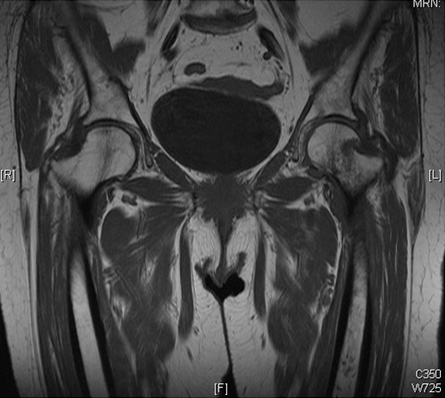 [Figure caption and citation for the preceding image starts]: Anteroposterior pelvic radiograph showing a possible intracapsular fracture of the left hipFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
[Figure caption and citation for the preceding image starts]: Anteroposterior pelvic radiograph showing a possible intracapsular fracture of the left hipFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends]. [Figure caption and citation for the preceding image starts]: Anteroposterior x-ray showing femoral neck fractureFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
[Figure caption and citation for the preceding image starts]: Anteroposterior x-ray showing femoral neck fractureFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends]. [Figure caption and citation for the preceding image starts]: Anteroposterior pelvic radiograph showing a left intracapsular fracture fixed with a sliding hip screw constructFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
[Figure caption and citation for the preceding image starts]: Anteroposterior pelvic radiograph showing a left intracapsular fracture fixed with a sliding hip screw constructFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends]. [Figure caption and citation for the preceding image starts]: Intramedullary nail (cephalomedullary) for the treatment of an unstable intertrochanteric fractureFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
[Figure caption and citation for the preceding image starts]: Intramedullary nail (cephalomedullary) for the treatment of an unstable intertrochanteric fractureFrom the collection of Bradley A. Petrisor, MSc, MD, FRCSC and Mohit Bhandari, MD, MSc, FRCSC [Citation ends].
Technetium bone scan may also be used if there is no access to an MRI or CT; however, the bone scan may be falsely negative for up to 72 hours from the time of injury.[50] False positives may also arise with bone scan, related to osteoarthritis, soft-tissue injury, or any other process that may increase bone turnover.[50]
Laboratory tests
Look for other medical conditions that need urgent treatment prior to surgery: for example, anaemia, diabetes, or abnormal electrolytes.[45]
Arrange the following blood tests:[46]
Full blood count
Anaemia is common in patients with hip fracture.[45][46] Anaemia is present in 50% of patients preoperatively.[73]
Symptomatic anaemia can cause dizziness on standing and general fatigue leading to falls.
Consider the cause of anaemia and possibility of underlying malignancy.[49] If the fracture is unexplained, consider a diagnosis of myeloma and arrange a full blood count and blood tests for calcium and plasma viscosity or erythrocyte sedimentation rate.[49] If serum free light chain testing is not available, use a Bence-Jones test to check for free light chains contained in urine.[49]
May require correction to optimise fitness for surgery.[45][60][74]
A haemoglobin concentration <80 g/L (<8 g/dL) may be a reason to delay surgery.[60] Acceptable levels will depend on patient factors. Consult local guidelines for when to transfuse.
Practical tip
Transfusion preoperatively may be needed when the patient has cardiorespiratory diseases or frailty, or is likely to lose a significant amount of blood during the procedure.
Urea/electrolytes
Electrolyte abnormalities are common and may contribute to falls risk (e.g., hyponatraemia, hypokalaemia).[45][46]
May require correction to optimise fitness for surgery.[74]
Acceptable levels will depend on patient factors.
Plasma sodium concentration <120 or >150 mmol/L (<120 or >150 mEq/L) and potassium concentration <2.8 or >6.0 mmol/L (<2.8 or >6.0 mEq/L) may be a reason to delay surgery.[60]
Glucose
Group and save
Patient is likely to need surgery.
Consider the patient’s baseline levels.
Consult your hospital’s guidelines on when a transfusion is required.
Coagulation screen
May be abnormal in chronic liver disease or if the patient has severe sepsis or multi-organ failure.
Follow local guidelines to reverse any coagulopathy prior to surgery.
Attend to a reversible coagulopathy so that it does not cause an unnecessary delay to surgery.[60]
ECG
Perform an ECG.[46]
Syncopal falls may result from a cardiac arrhythmia.
Review the ECG for signs of cardiac syncope, such as heart block, intraventricular conduction abnormalities, or inappropriate sinus bradycardia (40-50 bpm) or slow atrial fibrillation (40-50 bpm) in the absence of negatively chronotropic medications.[75]
Rarely cardiac syncope is due to tachycardia such as ventricular tachycardia.[75]
Look for evidence of ischaemic heart disease, such as ST changes or new left bundle branch block, and of prolonged QT interval.[75]
Patients may have an increased risk of arrhythmias due to underlying electrolyte abnormalities or anaemia.[45][46] It is important to treat these early to prevent any delay to surgery.
A correctable cardiac arrhythmia with a ventricular rate >120/minute may be a reason to delay surgery.[60]
Use a standardised and validated measure to check for cognitive impairment.[51][52] Cognitive impairment is associated with a high risk of falls.[42]
Delirium
Use the 4AT assessment for delirium.[52] In critical care or in the recovery room after surgery, use the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) or Intensive Care Delirium Screening Checklist (ICDSC) instead of the 4AT.[52]
The 4AT scores the patient on:
Alertness
Abbreviated mental test score
Attention
Acute change or fluctuation in cognition or mental function.
Signs of delirium include:[52]
Confusion and disorientation
Slow responses
Visual or auditory hallucinations
Agitation
Sleep disturbance
Lack of co-operation
Withdrawal
Changes in communication, mood, and/or attitude.
Hip fracture is a major risk factor for delirium.
Identify any other risk factors for delirium preoperatively, such as:[52]
Age 65 years or older
Cognitive impairment and/or dementia
An existing clinical condition that is deteriorating or at risk of deteriorating.
Look for reversible causes of delirium, such as:
Intercurrent illness
Urinary retention
Constipation.
Ask relatives/carers about the patient’s usual mental state and the presence of any of these indicators.
Practical tip
Delirium affects the patient’s capacity to give informed consent. Involve relatives/carers and encourage visitors to help re-orientate the patient.
Classify fractures radiographically into intracapsular and extracapsular to guide surgical management.
Intracapsular fractures
The retinacular vessels that pass up the femoral capsule may be damaged, especially if the fracture is displaced, resulting in poor blood supply to the femoral head often leading to avascular necrosis.[1]
Extracapsular fractures
Include trochanteric or subtrochanteric, which typically heal well.
Fractures may be further subdivided, depending on the level of the fracture and the presence or absence of displacement and comminution.[1]
The Garden classification categorises intracapsular hip fractures into four types based on anteroposterior radiographs of the hip. It incorporates displacement, fracture completeness, and relationship of bony trabeculae in the femoral head and neck.[3][4]
Intracapsular (femoral neck) fractures can be classified as follows:[5]
Type 1: impacted in valgus
Type 2: undisplaced
Type 3: displaced <50% and in varus
Type 4: completely displaced.
Reliability studies have suggested that there is poor inter- and intra-rater agreement in categorising fractures with this classification.[6]
Extracapsular fractures are classified broadly into trochanteric and subtrochanteric types.
The AO classification is useful in further guiding surgical management.[7] This categorises fractures according to location, joint involvement, fracture pattern, and geometry.
[Figure caption and citation for the preceding image starts]: Classification of hip fractures. Fractures in the blue area are intracapsular and those in the red and orange areas are extracapsularBMJ. 2006 Jul 1;333(7557):27-30 [Citation ends].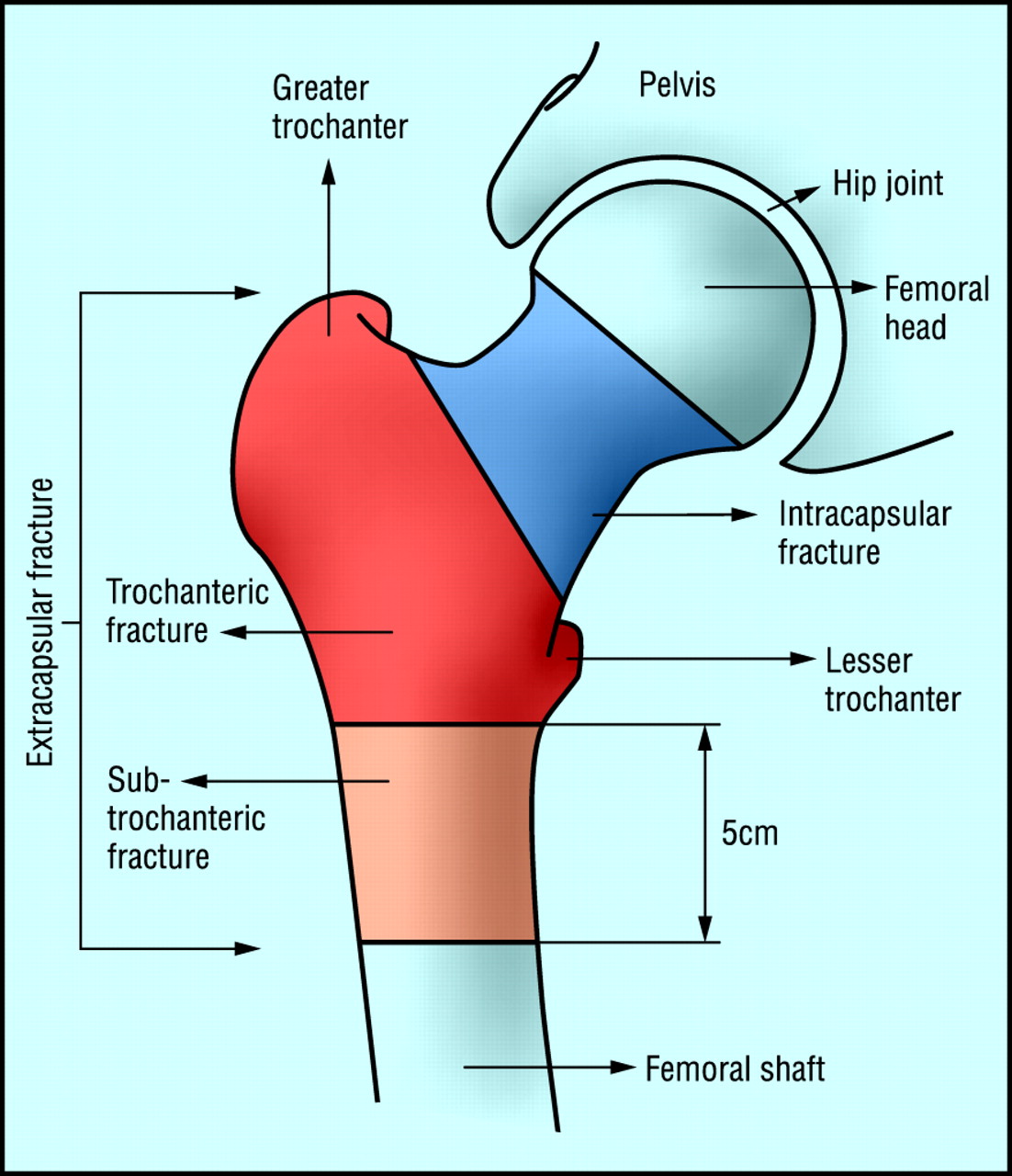
Use of this content is subject to our disclaimer