Approach
Your Organisational Guidance
ebpracticenet urges you to prioritise the following organisational guidance:
Klinische richtlijn rond lage rugpijn en radiculaire pijnPublished by: KCELast published: 2018Guide de pratique clinique pour les douleurs lombaires et radiculairesPublished by: KCELast published: 2018There are no typical characteristics in a patient's history that confirm or disprove the diagnosis of discogenic back pain.[62] Although suggestive, history and clinical examination findings are not conclusive. Correlation with radiological investigations is necessary to confirm the diagnosis of degenerative disc disease (DDD).
History
Detailed history is required to elicit possible secondary causes of low back pain (LBP). Red flags such as night pain, unexplained weight loss, fever, or symptoms of the gastrointestinal, urinary, and cardiorespiratory systems should always be part of the clinical assessment, as their presence may suggest an alternative diagnosis for back pain. Presentation with fever/chills, a history of IV drug abuse, or history of tuberculosis exposure may indicate the possibility of discitis. A known history of systemic malignancy is also a red flag. Patients with red flags should be imaged prior to any conservative treatment.
Features suggestive of discogenic LBP include a history of previous episode of acute pain or trauma and persistent LBP. The pain is frequently referred to the paraspinal muscles, buttocks, and the back of the thighs. Occasionally, there may be associated pain in a dermatomal distribution or in the groin or flank. Usually pain gets worse with axial loading (standing or sitting) and improves with recumbence.
Radicular leg pain can result from nerve root compression due to hypertrophied facet joints, disc prolapse, or foraminal narrowing due to loss of disc height or to instability at that motion segment. Radicular leg pain may range in severity from mild constant pain to excruciating pain. It is usually felt in the dermatomal distribution of the affected nerve root.
Neurological features such as saddle (perineal) anaesthesia, sphincteric dysfunction, bladder retention, and leg weakness suggest cauda equina syndrome. [Figure caption and citation for the preceding image starts]: MRI spine: degenerate facet joints and a large facet cyst from the left L5S1 facet joint compressing the left S1 nerve rootFrom the collection of Dr N. Quiraishi [Citation ends].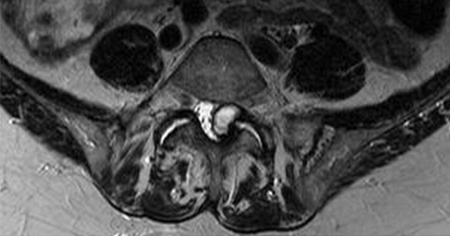 [Figure caption and citation for the preceding image starts]: MRI spine: degenerate L4-5 disc with a disc bulge and L5S1 disc with a high-intensity zoneFrom the collection of Dr N. Quiraishi [Citation ends].
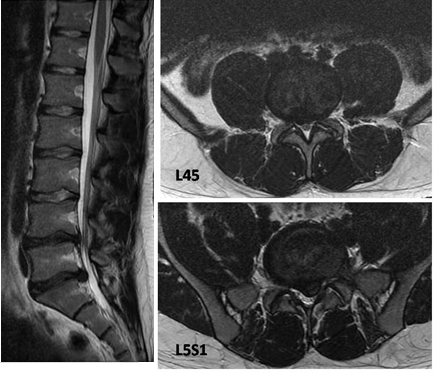
[Figure caption and citation for the preceding image starts]: MRI spine: degenerate L4-5 disc with a disc bulge and L5S1 disc with a high-intensity zoneFrom the collection of Dr N. Quiraishi [Citation ends]. [Figure caption and citation for the preceding image starts]: T2-weighted MRI spine: sagittal view (left) demonstrates degenerate discs; axial view (right) demonstrates left-sided L5S1 foraminal narrowingFrom the collection of Dr N. Quiraishi [Citation ends].
[Figure caption and citation for the preceding image starts]: T2-weighted MRI spine: sagittal view (left) demonstrates degenerate discs; axial view (right) demonstrates left-sided L5S1 foraminal narrowingFrom the collection of Dr N. Quiraishi [Citation ends].
Physical examination
The clinical examination of a patient with DDD is often unremarkable. Exacerbation of pain following pressure over the spinous process of the affected segment is considered as sign of discogenic pain by some clinicians.[63] Restriction in spinal flexion is related to paravertebral muscle spasm and results in reproduction of symptoms with subsequent easing of pain with extension. This appears to correlate with DDD in the absence of other spine pathology. Straight leg raise and other tests for radiculopathy are rarely positive; however, if the pain is reproduced by passively raising the extended leg (positive Lasegue sign), it is suggestive of compressive or inflammatory nerve root pathology.[64]
A neurological examination should assess limb strength and sensation. Neurological deficit is associated with a dysfunction of the nerve root and/or the cauda equina. This can be caused by advanced degenerative changes, although it is uncommon. A presumed diagnosis of cauda equina syndrome necessitates an urgent referral to the hospital.
A complete clinical examination should include the assessment of the abdomen and lower thorax to exclude intra-abdominal pathology (tumours, pancreatitis, aortic aneurysm) that may manifest with back pain.
Plain radiographs
Upright anteroposterior and lateral plain radiographs are a quick and simple investigation that may give valuable information; however, they are not routinely recommended for non-specific back pain.[65][66] Plain radiographs are recommended if recent significant trauma, osteoporosis, or age over 70 years.[66] For all other instances of LBP, such as spinal malignancy, infection, fracture, cauda equina syndrome, or ankylosing spondylitis or another inflammatory disorder, the preferred modality is lumbar magnetic resonance imaging (MRI).[66]
Plain radiographs show pathology much later than MRI and are not required for diagnosis of DDD. Degenerative changes (osteophytes, disc space narrowing, foraminal stenosis, endplate sclerosis, ligament calcification) may be seen if performed for other reasons.
Flexion/extension views of the lateral spine may be obtained to aid the diagnosis if there is a suspicion of spondylolisthesis (slippage of a vertebra on another) seen on plain radiographs.
MRI lumbar spine
MRI is the imaging study of choice for DDD due to its unique detail on the representation of the disc status.[64] A disc that appears normal on MRI is unlikely to be the pain generator, suggesting that additional investigations should be performed to identify the true cause of back pain. Important characteristics that should be examined are: signs of degeneration, evaluation of the disc height, the presence or absence of annular tears, and endplate changes.[67][68]
MRI findings should always be interpreted with caution because the presence of degenerative findings is not an absolute indicator of a cause of the patient's symptoms.[69][70][71][72][73] Many of the abnormalities detected on lumbar spine imaging are common in people who are asymptomatic and seem only to be loosely associated with back symptoms.
Modic changes
The decreased capacity of the disc to maintain hydration under load leads to uneven and increased stress concentrations along the endplate and the annulus during axial loading.[74] These changes may secondarily affect the local marrow environment of the vertebral body, resulting in endplate and bone marrow signal changes on MRI, also known as Modic changes.[68][75]
The correlation of these changes seen on different MRI sequences with the histopathological findings is known as Modic classification. Types 2 and 3 indicate chronic changes.
Type 1 - decreased signal intensity on T1-weighted MRI and an increased signal on T2-weighted images indicates acute or subacute inflammatory changes.
Type 2 - increased signal intensity on T1-weighted images and isointense or slightly increased signal on T2-weighted images indicates chronic repetitive trauma.
Type 3 - decreased signal activity on both T1- and T2-weighted imaging corresponds to advanced degeneration with reactive osteosclerosis.
The clinical importance of these findings is that they are characteristic for the presence of degenerative disc disease and can be distinguished from changes secondary to malignancy or osteomyelitis. Modic changes have also shown a positive correlation with age and disc degeneration.[75][76][77] However, the prevalence, and above all the association with LBP, vary greatly between studies.[78][79][80]
An association of Modic changes (most commonly type 2) with a chronic LBP is seen in 81% of patients.[81]
High-intensity zone (HIZ) lesions
Represent another MRI finding that has been correlated with symptomatic DDD.[82] They are described as MRI hyper-intense signal changes on T2-weighted images, located within the posterior annulus of the disc and visible on both axial and sagittal views. These well-defined changes, which can exhibit contrast enhancement, were present in 28% of patients with LBP, indicating a painful internal disc disruption.[82] These findings are in agreement with other studies that demonstrated even higher (80%) correlation between LBP and HIZ lesions.[83]
However, the significance of the HIZ has been questioned with regards to its low sensitivity for pain reproduction and, therefore, its usefulness.[5][84]
The controversy suggests that HIZ lesions are variably present in painful degenerative discs. They reflect entities as diverse as annular tears, trapped nucleus pulposus herniations, or even focal degenerative myxoid change within the outer annulus.[82][85][86] This heterogeneity explains why HIZ lesions have been shown inconsistent as sensitive markers for discogenic pain.[87][88][Figure caption and citation for the preceding image starts]: T2-weighted MRI spine: sagittal view (left) demonstrates 2 level disc dehydration at L4-5 and L5S1 with a moderate reduction in disc height; axial views (right) demonstrate constitutionally narrow canal at L4-5 with a moderate disc prolapse and a large disc prolapse at L5S1 level with left S1 root compressionFrom the collection of Dr N. Quiraishi [Citation ends].
 [Figure caption and citation for the preceding image starts]: MRI spine: degenerate L4-5 disc with a disc bulge and L5S1 disc with a high-intensity zoneFrom the collection of Dr N. Quiraishi [Citation ends].
[Figure caption and citation for the preceding image starts]: MRI spine: degenerate L4-5 disc with a disc bulge and L5S1 disc with a high-intensity zoneFrom the collection of Dr N. Quiraishi [Citation ends].
CT spine imaging (CT scan, SPECT, CT myelogram)
Computed tomography (CT) scan is a useful modality to obtain a better assessment of the bony anatomy, especially in the presence of a previous operation.[64] The presence of metal causes artifacts on an MRI scan, making assessment of the underlying pathology difficult. Assessment of a fusion and the location of the metal work is best performed by CT scan.
The CT scan capabilities can be enhanced by way of an associated bone scan (Single Photon Emission Computed Tomography [SPECT]). SPECT locates pathologies that cause an increased blood flow locally (facet joint inflammation, discitis, neoplastic lesions). This is useful when other imaging modalities are negative but pathology (not necessarily discogenic) is still suspected. It is not a routine primary diagnostic tool.
CT myelogram provides visual assessment of the spinal canal and the neural foramina.[64] It combines the CT assessment after the instillation of a water soluble radio-opaque contrast in the cerebrospinal fluid. This allows for a better assessment of the stenotic segments in the spinal canal and the nerve root foramen. Although traditional CT scans are performed in the supine position, myelograms can be performed with the patient upright. A myelogram is an invasive investigation and involves injection of a contrast material into the epidural space. It is not commonly performed, though it is a useful adjunct to CT scans in the case of revision setting, in the presence of previously placed implants, and in situations where an MRI is contraindicated (e.g., cardiac pacemakers, brain and dorsal column stimulators).
Discography or MRI with gadolinium (contrast) enhancement
Provocation discography is the only imaging technique that involves direct stimulation of the disc. Plain radiographs are taken as the initial step. The test then consists of 2 components:
reproduction of the pain (concordant pain) by increasing the intradiscal pressure by injecting the affected disc with a contrast material
painless discogram in the adjacent normal discs (control levels).
The procedure is regarded to be positive when there is subjective reproduction of the patient's pain at the injected (pathological) level and no or minimal pain response when the 2 adjacent or control levels are injected.[89][90] Radiographs showing leakage of dye through the annulus fibrosus suggests advanced disease and adds credence to the discography. The main limitation of the procedure is its reliance on subjective pain responses from the patient.
Although not a routine test in most units, discography could be combined with a CT scan to provide for a CT discogram to assess the annular degenerative pattern. This also provides for a grading system of annular tears.
Grade I: normal cotton ball pattern; no extension beyond central half of disc
Grade II: normal lobular pattern; no extension beyond central half of disc
Grade III: fissured extension to inner annulus; no disc protrusion
Grade IV: degeneration + extension to outer annulus; may include disc protrusion
Grade V: degeneration past annular extension; definite protrusion + possible disc fragment.
Suitable candidates for discography are patients with chronic LBP (>3 months), those who have not been improved by conservative treatment or other minimally invasive procedures (facet joint injections, nerve root block, sacroiliac injections), and patients who are candidates for a possible interventional treatment aimed at reducing the discogenic pain.
Contraindications for the procedure include: infection (at the injection site or systemic), pregnancy, allergy to contrast, and haemorrhagic coagulopathy or use of anticoagulants.
Although provocation discography aids the diagnosis of symptomatic intervertebral disc disease, the procedure itself can damage the disc and cause additional degenerative disc disease.[91][92]
As an alternative, the use of MRI with gadolinium (contrast) enhancement may be considered. This is administered by IV and causes enhancement of the oedematous, scarring structures on T1-weighted images, differentiating more accurately the presence of scarring tissue that forms within a healing full-thickness annular tear.[Figure caption and citation for the preceding image starts]: Discography: a patient presents with back and right leg pain that did not respond to a trial of conservative management. MRI (left, sagittal T2-weighted image) demonstrates multiple degenerate discs with loss of normal hydration, reduced signal, and loss of the nuclear-annular transition, with a normal disc height. A 3-level discography at L3-4, L4-5, and L5S1 (middle, AP radiograph; right, lateral radiograph) reveals a low-pressure injection with degenerate annular tears at all 3 levels, with 5/5 pain concordance at L5S1; 3/5 at L4-5; and 0/5 at L3-4From the collection of Dr N. Quiraishi [Citation ends].
Emerging investigations
Genetic testing
Genes associated with disc degeneration include the genes that code for collagen I (COL9A2), collagen IX (COL9A3), collagen XI (COL11A2), interleukin 1 (IL-1), interleukin 6 (IL-6), aggrecan (AGC1), vitamin D receptor (VDR), metalloproteinases (MMP-3), and cartilage intermediate layer protein (CILP).
Testing is currently under development and not available for routine clinical use.
Functional spinal imaging
Includes magnetic resonance spectroscopy; MRI with mapping T2 relaxation time; mapping T1 rho; dynamic MRI; diffusion imaging.
Testing is currently under development and not available for routine clinical use.
Use of this content is subject to our disclaimer