History and exam
Your Organisational Guidance
ebpracticenet urges you to prioritise the following organisational guidance:
Évaluation du risque cardiovasculaire en première lignePublished by: Domus MedicaLast published: 2010Cardiovasculaire risicobepaling in de eerste lijnPublished by: Domus MedicaLast published: 2020Évaluation du risque cardiovasculaire en première lignePublished by: Domus MedicaLast published: 2020Key diagnostic factors
common
presence of risk factors
Key risk factors include excess body weight, type 2 diabetes mellitus, hypothyroidism, and cholestatic liver disease.
family history of early onset of coronary heart disease or dyslipidaemia in first-degree relatives
Given the paucity of early signs and symptoms of hypercholesterolaemia, it is crucial to perform a thorough family history. A significant family history (for example, of early onset coronary heart disease [e.g., occurring in male first-degree relatives under 55 years old and in female first-degree relatives under 60-65 years old]) suggests primary hypercholesterolaemia.[41][44]
history of cardiovascular disease
Most patients with hypercholesterolaemia are not diagnosed until premature cardiovascular disease becomes symptomatic.
It is important to assess lipid profiles in patients presenting with angina, myocardial infarction, stroke, and peripheral vascular disease.
consumption of saturated fats and trans-fatty acids
Sedentary lifestyle and a diet characterised by excessive consumption of saturated fats, and trans-fatty acids.[14]
excess body weight (especially abdominal obesity)
xanthelasmas
Yellow plaques that occur most commonly near the inner canthus of the eyelid.[Figure caption and citation for the preceding image starts]: Extravascular lipid deposits (xanthelasma) (arrows) in a patient treated with margarine enriched in plant sterolsVergès B, Athias A, Petit J-M, et al. Extravascular lipid deposit (xanthelasma) induced by a plant sterol-enriched margarine. BMJ Case Reports. 2009;2009:bcr10.2008.1108 [Citation ends].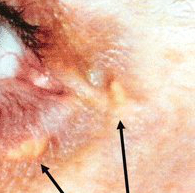
Half of these lesions are associated with elevated plasma lipid levels.[45]
Some occur with altered lipoprotein composition or structure, such as lowered high-density lipoprotein cholesterol levels.
They frequently occur in patients with type II and IV hyperlipidaemia.
uncommon
tendinous xanthomas
Slowly enlarging subcutaneous nodules related to the tendons or the ligaments.
The extensor tendons of the hands, feet, and Achilles tendons are the most common locations. A relationship to previous trauma to the site often exists.[Figure caption and citation for the preceding image starts]: Xanthomata of the Achilles' tendonCenter for Preventive Cardiology, University of Maryland Medical Center [Citation ends]. [Figure caption and citation for the preceding image starts]: Xanthomata over the metacarpophalangeal jointsCenter for Preventive Cardiology, University of Maryland Medical Center [Citation ends].
[Figure caption and citation for the preceding image starts]: Xanthomata over the metacarpophalangeal jointsCenter for Preventive Cardiology, University of Maryland Medical Center [Citation ends].
Associated with severe hypercholesterolaemia and elevated low-density lipoprotein cholesterol levels (familial hypercholesterolaemia). They are also associated with some of the secondary hyperlipidaemias, such as cholestasis.
Other diagnostic factors
uncommon
arcus cornealis with onset before the age of 45 years
White or grey opaque ring in the corneal margin.
The result of cholesterol deposits in the hyalinosis of the corneal stroma; can be seen in patients with ocular defects or familial hyperlipidaemia.
tuberous xanthomas
Firm, painless, red-yellow nodules.
Multilobulated tumours can develop once individual lesions coalesce.
Usually related to pressure areas, such as the extensor surfaces of the knees, elbows, and buttocks.
Particularly associated with hypercholesterolaemia and increased levels of low-density lipoprotein. They can be associated with familial dysbetalipoproteinaemia and familial hypercholesterolaemia, and they may be present in some of the secondary hyperlipidaemias.
Risk factors
strong
insulin resistance and type 2 diabetes mellitus
Hypercholesterolaemia due to increased very low-density lipoprotein cholesterol (VLDL-C) and expressed by high total cholesterol and non-high-density lipoprotein cholesterol (non-HDL-C) but not low-density lipoprotein cholesterol (LDL-C) can be seen in the context of mixed dyslipidaemia, and is associated with insulin resistance.[21]
LDL-C levels are not increased in insulin resistance. However, the number of apolipoprotein B-containing lipoproteins, such as VLDL-C, is increased. HDL-C and the number of apolipoprotein A-I particles are usually reduced in insulin resistance. A correlation exists between severity of insulin resistance and degree of lipoprotein abnormalities: greater degrees of insulin resistance are associated with increased VLDL production, reduced clearance, larger VLDL particles, and smaller LDL and HDL particles.[22]
The total number of LDL, intermediate-density lipoprotein, and VLDL particles is also increased in patients with insulin resistance.
excess body weight (body mass index >25 kg/m²)
Weight gain is associated with increased low-density lipoprotein (LDL) cholesterol levels. However when abdominal obesity is present, it is associated with a variety of unfavourable changes in lipid metabolism, similar to those found in insulin resistance and type 2 diabetes.[22][23] This includes a waist circumference that is >94 cm in white and black men, >80 cm in white and black women, >90 cm in Asian men, and >80 cm in Asian women.[23][24]
Loss of body fat may partially reverse hypercholesterolaemia and hypertriglyceridaemia.
hypothyroidism
In a study of patients with primary hypothyroidism, 56% had isolated hypercholesterolaemia and another 34% had combined hypercholesterolaemia with hypertriglyceridaemia.[28]
In another study of patients referred to a lipid disorder speciality clinic, the rate of overt hypothyroidism was found to be 2.8%, and 4.4% of patients had subclinical hypothyroidism.[29]
The severity of lipid abnormalities increases with the severity of the hypothyroidism.
Because of this association, it is appropriate to assess thyroid-stimulating hormone in any patient presenting with dyslipidaemia.
cholestatic liver disease
Lipoprotein-X (an abnormal low-density lipoprotein in cholestatic conditions) plays a major role in the pathogenesis of hypercholesterolaemia observed with primary biliary cirrhosis and similar hepatic disorders.
In these disorders, serum cholesterol concentrations may exceed 12.95 mmol/L (500 mg/dL) and physical stigmata such as xanthomas may be found.
weak
cigarette smoking
Patients smoking 2 packs of cigarettes per day had a mild reduction of high-density lipoprotein cholesterol.[25] This reduction may be more pronounced in the setting of concomitant alcohol intake.[26]
It has been suggested that smoking may induce insulin resistance, with associated increases in the size and number of low-density lipoprotein and very low-density lipoprotein particles.[27]
nephrotic syndrome
Hyperlipidaemia observed in patients with nephrotic syndrome is partially due to a reduction in lipid catabolism. The low oncotic pressure seen in these patients is thought to lead to increased hepatic synthesis of lipoproteins.
use of certain drugs
Mild alterations of lipid metabolism can occur with drug therapy for other medical conditions. The mechanisms for this differ in each drug class.
Drugs commonly implicated are high-dose thiazide diuretics, oral oestrogens, glucocorticoids, anabolic steroids (also reduce high-density lipoprotein cholesterol), and atypical antipsychotics, such as olanzapine and clozapine.
The use of protease inhibitors in patients living with HIV is associated with a class-related adverse effect termed lipodystrophy syndrome, which has marked abnormalities of lipid and glucose metabolism.
Isotretinoin (a retinoid) is also associated with hypercholesterolaemia and hypertriglyceridaemia.
Use of this content is subject to our disclaimer