Approach
Rickettsial diseases are difficult to diagnose. Diagnosis is usually based on the presence of a fever, rash, and eschar. However, the clinical presentation can vary. It is important to recognise that other life-threatening illnesses such as meningococcal disease can have similar signs and symptoms and should be considered in the diagnostic work up, and treated empirically as appropriate.[22]
Rickettsial infections are relatively common infections in travellers returning from tropical or developing countries. In most febrile returned travellers, malaria should be considered first and ruled out before considering other causes. Once malaria is ruled out, rickettsial infection should be considered along with other potential differential diagnoses.
Rickettsial infections are a notifiable disease in some countries.
History
In scrub typhus and spotted fever group rickettsial infections, the patients are normally healthy people, often travellers from the tropics, who have become unwell on returning to their country of origin. They may or may not recall having been "bitten by something". They have often been in heavily vegetated regions and exposed to trees, jungle, scrub, or bush and sometimes to animals such as dogs, cats, and wildlife. The classic story is of having returned from a game safari in Africa. However, rickettsial infections are found worldwide.[23]
For typhus group rickettsial infection the patients are often very poor, homeless people living on the streets of major cities. They may have human body lice or they may live in poor circumstances where they are exposed to rodents and rodent flea faeces. Their clothing may be infested with the human body louse.[23]
Clinical presentation
Clinical presentations vary with the causative agent and patient.[23] Patients usually present with a fever and may have a rash (usually maculopapular) and an eschar (the bite site of the ectoparasite). The eschar may be well hidden, for example in the hair, in the groin, under breasts, or in the natal cleft. The patient usually complains of severe headache, general myalgia, nausea/vomiting, abdominal pain, and marked fatigue. Patients often have hepatosplenomegaly and may be tachypnoeic or encephalopathic.[23][22] Arthralgia is less common.
If the patient presents early in the illness, the rash may not yet be present. In people with darker skin the rash may be difficult to see. When present, the rash is usually macular or papular but in some rickettsial infections may be vesicular (e.g., Queensland tick typhus due to Rickettsia australis and rickettsial pox due to R akari) or petechial (e.g., epidemic typhus due to R prowazekii).[Figure caption and citation for the preceding image starts]: Characteristic rash (in this case caused by Rocky Mountain spotted fever)CDC Public Health Image Library [Citation ends].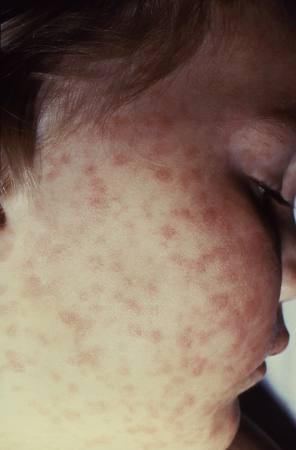
Whether an eschar is present or not is highly variable from patient to patient, from geographic place to place, and varies according to the Rickettsia species or Orientia tsutsugamushi strain involved. The lymph nodes draining the eschar may be enlarged.
Initial investigations
Rickettsial diseases require early diagnosis and treatment to prevent severe outcomes. Molecular and serological testing are the most commonly available methods for confirming the diagnosis.
Full blood count:
Decreasing platelet count (thrombocytopenia) is common. It may be mild or severe, but is usually present during acute rickettsial infections. Leukocyte levels may be low, normal, or raised. Lymphocytes may be atypical in morphology, as is sometimes seen in viral infections.
Serum electrolyte levels:
Usually show hyponatraemia.
Liver function tests:
Transaminases are usually slightly elevated.
Inflammatory markers (e.g., C-reactive protein):
These are significantly raised in rickettsial diseases.
Rickettsial serology:
May be negative early in the infection but will serve as a control for a further (convalescent) serum taken later in the illness or on recovery. The two sera will normally show seroconversion. If the initial serum is already seropositive for rickettsiae, the later serum will show a significant rise in antibody titres. Both of these serological patterns are diagnostic of rickettsial infection. Serology will differentiate the three rickettsial infection groups (spotted fever group, typhus group, and scrub typhus group), but will not indicate the species of the rickettsia infecting the patient.[24]
Polymerase chain reaction (PCR):
This is best done on a swab or biopsy of the eschar (if present). These samples must be sent to a reference laboratory as this requires a specific PCR assay. If done on blood, the test may give a false-negative result during the first several days of illness.[25]
Early diagnosis may be difficult with serology, and there is some emerging evidence to suggest there is a place for combining nucleic acid amplification testing with serology to improve accuracy and allow for earlier detection.[26]
Other investigations
Cell cultures:
Growth of rickettsia from blood (during the early rickettsaemic phase) or from an eschar biopsy. These samples must be sent to a reference laboratory for inoculation of cell cultures.[25]
Biopsy of eschar for immunohistochemistry:
This sample must be sent to a reference laboratory for staining with specific anti-rickettsial antisera.
Therapeutic trial:
All rickettsiae respond to doxycycline, so a therapeutic trial is often useful, although it is not a specific intervention as other infections will also respond well to treatment with doxycycline.
Chest x-ray:
Only order if clinically indicated (e.g., pneumonia suspected). May be positive in murine typhus (Rickettsia typhi) and scrub typhus (Orientia tsutsugamushi).
Use of this content is subject to our disclaimer