Pleural mesothelioma is a rare malignancy and can be overlooked as a possible cause of dyspnoea or pleural effusion. History of asbestos exposure associated with a pleural effusion is strongly suggestive; however, the absence of asbestos exposure on history does not exclude this diagnosis.
Patients may be asymptomatic and present with an incidental finding of pleural abnormalities on diagnostic imaging studies.
Clinical presentation
A careful social history, enquiring about possible asbestos exposure (at least occupational), including source and dates of exposure, is crucial. Occupational history regarding the type of work performed (shipyard; construction; maintenance; vehicle brake mechanic; asbestos cement; insulation; or production of tiles, shingles, gaskets, brakes, or textiles) may provide some clues. Men are predominantly affected (male to female ratio 3:1) and as the latency period between exposure to asbestos and development of pleural mesothelioma is 20-40 years, patients are typically older adults in their sixth to ninth decade of life.[4]National Cancer Institute. Mesothelioma: recent trends in SEER age-adjusted incidence rates, 2000-2022. Apr 2025 [internet publicaton].
https://seer.cancer.gov/statistics-network/explorer/application.html?site=111&data_type=1&graph_type=2&compareBy=sex&chk_sex_1=1&chk_sex_3=3&chk_sex_2=2&rate_type=2&race=1&age_range=1&stage=101&advopt_precision=1&advopt_show_ci=on&hdn_view=1&advopt_show_apc=on&advopt_display=1#resultsRegion1
[11]Price B, Ware A. Mesothelioma trends in the United States: an update based on Surveillance, Epidemiology, and End Results Program data for 1973 through 2003. Am J Epidemiol. 2004 Jan 15;159(2):107-12.
https://academic.oup.com/aje/article/159/2/107/166453
http://www.ncbi.nlm.nih.gov/pubmed/14718210?tool=bestpractice.com
Symptoms are usually related to the presence of intrathoracic disease and include shortness of breath; dry, non-productive cough; and chest pain. Non-specific symptoms, such as fatigue, fever, sweats, and weight loss, are also common. A history of abdominal distension and/or pain is more typical of primary peritoneal mesothelioma, but may also denote intra-abdominal extension from advanced pleural disease.
Physical findings suggestive of a pleural effusion are typical. These include decreased breath sounds and dullness to percussion on the affected side. Decreased breath sounds can also indicate trapped lung or bronchial obstruction, both of which may be caused by pleural mesothelioma.
Imaging studies
When mesothelioma is suspected, imaging studies should be obtained.
Chest x-ray (CXR)
Most useful in the differential diagnosis, CXR is recommended as initial imaging for patients with relevant symptoms and signs (e.g., dyspnoea, chest pain, and weight loss).[43]American College of Radiology. ACR appropriateness criteria: chronic dyspnea-noncardiovascular origin. 2024 [internet publication].
https://acsearch.acr.org/docs/69448/Narrative
[44]Woolhouse I, Bishop L, Darlison L, et al. British Thoracic Society guideline for the investigation and management of malignant pleural mesothelioma. Thorax. 2018 Mar;73(suppl 1):i1-30.
https://www.brit-thoracic.org.uk/quality-improvement/guidelines/mesothelioma
http://www.ncbi.nlm.nih.gov/pubmed/29444986?tool=bestpractice.com
[45]Popat S, Baas P, Faivre-Finn C, et al. Malignant pleural mesothelioma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2022 Feb;33(2):129-42.
https://www.annalsofoncology.org/article/S0923-7534(21)04820-1/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/34861373?tool=bestpractice.com
[46]National Institute for Health and Care Excellence. Suspected cancer: recognition and referral. Apr 2025 [internet publication].
https://www.nice.org.uk/guidance/ng12/chapter/Recommendations-organised-by-site-of-cancer
Possible findings associated with mesothelioma include unilateral pleural effusion, pleural thickening, reduced lung volumes, or parenchymal changes related to asbestos exposure (e.g., lower zone linear interstitial fibrosis, pleural calcification). CXR use is limited by poor visualisation of the pleura (that will miss subtle abnormalities).[43]American College of Radiology. ACR appropriateness criteria: chronic dyspnea-noncardiovascular origin. 2024 [internet publication].
https://acsearch.acr.org/docs/69448/Narrative
[Figure caption and citation for the preceding image starts]: Chest x-ray demonstrating total left-sided collapse and replacement of hemithorax with mesothelioma; there is reduced expansion on this sideFrom BMJ Case Reports 2011;doi:10.1136/bcr.09.2010.3319 [Citation ends].
UK guidance recommends referral for urgent CXR (within 2 weeks) when people aged 40 years and older present with at least two symptoms consistent with cancer (cough, fatigue, shortness of breath, chest pain, weight loss, appetite loss) or at least one symptom and a history of either smoking or asbestos exposure.[46]National Institute for Health and Care Excellence. Suspected cancer: recognition and referral. Apr 2025 [internet publication].
https://www.nice.org.uk/guidance/ng12/chapter/Recommendations-organised-by-site-of-cancer
X-ray is also appropriate in patients with finger clubbing or clinical signs of pleural disease.[46]National Institute for Health and Care Excellence. Suspected cancer: recognition and referral. Apr 2025 [internet publication].
https://www.nice.org.uk/guidance/ng12/chapter/Recommendations-organised-by-site-of-cancer
Computed tomography (CT)
If clinical suspicion is high, CT scan of the chest and upper abdomen with intravenous contrast should be obtained for diagnosis and initial staging of mesothelioma.[44]Woolhouse I, Bishop L, Darlison L, et al. British Thoracic Society guideline for the investigation and management of malignant pleural mesothelioma. Thorax. 2018 Mar;73(suppl 1):i1-30.
https://www.brit-thoracic.org.uk/quality-improvement/guidelines/mesothelioma
http://www.ncbi.nlm.nih.gov/pubmed/29444986?tool=bestpractice.com
[46]National Institute for Health and Care Excellence. Suspected cancer: recognition and referral. Apr 2025 [internet publication].
https://www.nice.org.uk/guidance/ng12/chapter/Recommendations-organised-by-site-of-cancer
[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
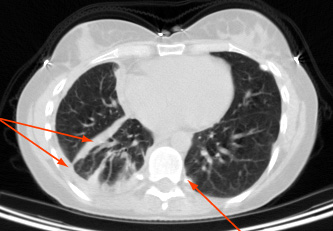
Findings suggesting a malignant process include circumferential or nodular pleural thickening or involvement of the mediastinal pleura.[48]Leung AN, Müller NL, Miller RR. CT in differential diagnosis of diffuse pleural disease. AJR Am J Roentgenol. 1990 Mar;154(3):487-92.
https://www.ajronline.org/doi/pdf/10.2214/ajr.154.3.2106209
http://www.ncbi.nlm.nih.gov/pubmed/2106209?tool=bestpractice.com
However, differentiating benign from malignant pleural abnormalities with CT alone is not reliable.
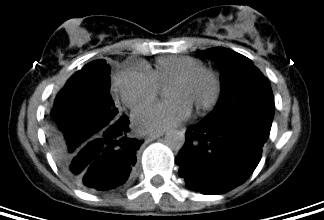
[Figure caption and citation for the preceding image starts]: Computed tomography scan of the lung showing a right-sided pleural mesothelioma and left-sided calcified pleural plaqueFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].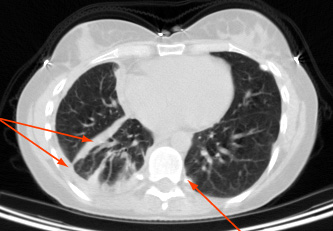 [Figure caption and citation for the preceding image starts]: Computed tomography scan of the mediastinum showing a right-sided pleural mesothelioma and left-sided calcified pleural plaqueFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Computed tomography scan of the mediastinum showing a right-sided pleural mesothelioma and left-sided calcified pleural plaqueFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].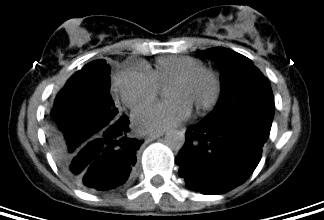
The optimal approach to mesothelioma measurement requires a radiologist to identify measurement sites on CT, per modified RECIST 1.1 criteria for mesothelioma.[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
[49]Armato SG 3rd, Nowak AK. Revised modified response evaluation criteria in solid tumors for assessment of response in malignant pleural mesothelioma (version 1.1). J Thorac Oncol. 2018 Jul;13(7):1012-21.
https://www.jto.org/article/S1556-0864(18)30596-3/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/29753121?tool=bestpractice.com
Positron emission tomography/computed tomography (PET/CT)
Used to help with initial staging and in the evaluation of pleural metastases.[43]American College of Radiology. ACR appropriateness criteria: chronic dyspnea-noncardiovascular origin. 2024 [internet publication].
https://acsearch.acr.org/docs/69448/Narrative
[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
PET/CT can distinguish benign pleural abnormalities from malignant processes.[50]Wang ZJ, Reddy GP, Gotway MB, et al. Malignant pleural mesothelioma: evaluation with CT, MR imaging, and PET. Radiographics. 2004 Jan-Feb;24(1):105-19.
https://pubs.rsna.org/doi/full/10.1148/rg.241035058
http://www.ncbi.nlm.nih.gov/pubmed/14730040?tool=bestpractice.com
PET/CT can be omitted when surgical resection is not being considered.[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
Chest magnetic resonance imaging (MRI)
Not recommended for initial imaging. Chest MRI, preferably with intravenous contrast, is used to resolve ambiguous findings on CT and to assess tumour invasion into the diaphragm, chest wall, mediastinum, and other areas.[43]American College of Radiology. ACR appropriateness criteria: chronic dyspnea-noncardiovascular origin. 2024 [internet publication].
https://acsearch.acr.org/docs/69448/Narrative
[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
[51]Katz SI, Straus CM, Roshkovan L, et al. Considerations for imaging of malignant pleural mesothelioma: a consensus statement from the International Mesothelioma Interest Group. J Thorac Oncol. 2023 Mar;18(3):278-98.
https://www.jto.org/article/S1556-0864(22)01928-1/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/36549385?tool=bestpractice.com
MRI is not as reliable as biopsy and will seldom alter management.
Confirming the diagnosis and prognostication
The diagnosis of mesothelioma cannot be made from imaging studies alone.
Thoracentesis
A thoracentesis is performed when a patient presents with clinically symptomatic pleural effusion or imaging studies confirm pleural effusion, with or without other pleural abnormalities. Important to determine whether the fluid is a transudate or exudate, and to obtain pleural fluid for cytological examination.[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
The sensitivity of cytology for mesothelioma is relatively low and often requires further pathological assessment of biopsied tissues.[52]Renshaw AA, Dean BR, Antman KH, et al. The role of cytologic evaluation of pleural fluid in the diagnosis of malignant mesothelioma. Chest. 1997 Jan;111(1):106-9.
http://www.ncbi.nlm.nih.gov/pubmed/8996002?tool=bestpractice.com
Biopsy
Biopsies of suspicious sites can confirm the diagnosis and are important for planning antineoplastic treatment.[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
They improve clinical staging, confirm the histological diagnosis and subtype (epithelioid, sarcomatoid, biphasic), and provide material for further studies, such as molecular profiling.[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
When performing a biopsy, aim to do so at the site intended for subsequent definitive resection to reduce the risk of implantation in the chest wall.[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
Pleural biopsies performed during video-assisted thoracoscopic surgery (VATS) exploration are recommended.[45]Popat S, Baas P, Faivre-Finn C, et al. Malignant pleural mesothelioma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2022 Feb;33(2):129-42.
https://www.annalsofoncology.org/article/S0923-7534(21)04820-1/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/34861373?tool=bestpractice.com
[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
Aim to limit the number of incisions to less than two.[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
When initial PET/CT or CT suggests contralateral disease, thoracoscopic biopsy can be used for confirmation.[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
Open pleural biopsy, using the smallest incision possible (ideally ≤6 cm), is reserved for when the thoracoscopic approach is not possible.[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
Histology
Histological assessment aims to confirm the pathological diagnosis by establishing that the lesion meets three criteria:[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: mesothelioma: pleural [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
It is diffuse (more aggressive) and not solitary (usually has a different pathogenesis and a less aggressive course)
It is mesothelial in origin (i.e., exclude other carcinomas with symptom overlap)
It is malignant and not reactive (i.e., presence of invasion into adjacent tissue, full-thickness serosal involvement, formation of expansile nodules).
Immunohistochemistry
Recommended for pathological diagnosis of all primary diagnoses.[44]Woolhouse I, Bishop L, Darlison L, et al. British Thoracic Society guideline for the investigation and management of malignant pleural mesothelioma. Thorax. 2018 Mar;73(suppl 1):i1-30.
https://www.brit-thoracic.org.uk/quality-improvement/guidelines/mesothelioma
http://www.ncbi.nlm.nih.gov/pubmed/29444986?tool=bestpractice.com
[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
Studies should use:[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: mesothelioma: pleural [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
[53]Shield PW, Koivurinne K. The value of calretinin and cytokeratin 5/6 as markers for mesothelioma in cell block preparations of serous effusions. Cytopathology. 2008 Aug;19(4):218-23.
http://www.ncbi.nlm.nih.gov/pubmed/17916095?tool=bestpractice.com
[54]Chu PG, Weiss LM. Expression of cytokeratin 5/6 in epithelial neoplasms: an immunohistochemical study of 509 cases. Mod Pathol. 2002 Jan;15(1):6-10.
http://www.ncbi.nlm.nih.gov/pubmed/11796835?tool=bestpractice.com
selected immunohistochemistry markers expected to be positive in mesothelioma (i.e., calretinin, cytokeratin 5/6, D2-40, and nuclear WT1), and
immunohistochemistry markers expected to be negative in mesothelioma (i.e., carcinoembryonic antigen [CEA], epithelial cell adhesion molecule, claudin 4, and thyroid transcription factor-1 [TTF-1]).
Other immunohistochemistry markers can be used to help to exclude differential diagnoses, diagnose mesothelioma, or guide prognosis (e.g., BAP1, MTAP, CDKN2A/p16).[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: mesothelioma: pleural [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
Patients with an epithelioid mesothelioma subtype, together with loss of BAP1 and retained p16 expression, have prolonged survival.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: mesothelioma: pleural [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
Potential diagnostic biomarkers, including soluble mesothelin-related peptides (SMRP), cannot be used alone to confirm pleural mesothelioma.[44]Woolhouse I, Bishop L, Darlison L, et al. British Thoracic Society guideline for the investigation and management of malignant pleural mesothelioma. Thorax. 2018 Mar;73(suppl 1):i1-30.
https://www.brit-thoracic.org.uk/quality-improvement/guidelines/mesothelioma
http://www.ncbi.nlm.nih.gov/pubmed/29444986?tool=bestpractice.com
[45]Popat S, Baas P, Faivre-Finn C, et al. Malignant pleural mesothelioma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2022 Feb;33(2):129-42.
https://www.annalsofoncology.org/article/S0923-7534(21)04820-1/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/34861373?tool=bestpractice.com
[55]US Food & Drug Administration. Fujirebio Mesomark assay. Humanitarian device exemption (HDE). H060004. Jan 2007 [internet publication].
https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfhde/hde.cfm?id=H060004
[56]Zhu M, Lu Z, Guo H, et al. Diagnostic value of combination of biomarkers for malignant pleural mesothelioma: a systematic review and meta-analysis. Front Oncol. 2023;13:1136049.
https://www.doi.org/10.3389/fonc.2023.1136049
http://www.ncbi.nlm.nih.gov/pubmed/37114132?tool=bestpractice.com
Germline testing
All patients with mesothelioma should be offered germline testing with appropriate pretest genetic counselling.[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
Pathogenic or likely pathogenic germline variants in BAP1 are associated with improved survival in patients with mesothelioma.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: mesothelioma: pleural [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
BAP1, a tumour suppressor, is implicated in the pathogenesis of not only mesothelioma but also uveal melanoma, cholangiocarcinoma, and clear cell renal cell carcinoma.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: mesothelioma: pleural [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
Patients with a positive germline testing result should be screened for these secondary cancers and their relatives should be offered genetic counselling.[2]National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: mesothelioma: pleural [internet publication].
https://www.nccn.org/professionals/physician_gls/default.aspx
[47]Kindler HL, Ismaila N, Bazhenova L, et al. Treatment of pleural mesothelioma: ASCO guideline update. J Clin Oncol. 2025 Mar 10;43(8):1006-38.
https://ascopubs.org/doi/10.1200/JCO-24-02425
http://www.ncbi.nlm.nih.gov/pubmed/39778125?tool=bestpractice.com
Additional studies
Once a diagnosis of mesothelioma is made, additional tests may be necessary to inform prognosis and guide management.
In patients who are considered for surgical resection, pulmonary function tests, echocardiogram, and mediastinoscopy are performed to assess cardiopulmonary function and to exclude metastases in the paratracheal and subcarinal lymph nodes within the mediastinum.
Routine blood work, including full blood count and basic metabolic panel, is necessary to establish baseline function before treatment.[Figure caption and citation for the preceding image starts]: Positron emission tomography scan showing hypermetabolic right-sided pleural mesotheliomaFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].

 [Figure caption and citation for the preceding image starts]: Computed tomography scan of the mediastinum showing a right-sided pleural mesothelioma and left-sided calcified pleural plaqueFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Computed tomography scan of the mediastinum showing a right-sided pleural mesothelioma and left-sided calcified pleural plaqueFrom the collection of Dr Chris R. Kelsey; used with permission [Citation ends].