Approach
Your Organisational Guidance
ebpracticenet urges you to prioritise the following organisational guidance:
Kanker van de mondholte: diagnose, behandeling en follow-upPublished by: KCELast published: 2015Cancers de la cavité buccale : diagnostic, traitement et suiviPublished by: KCELast published: 2015Oral pain and weight loss in a person aged >40 years with a strong smoking and drinking history should alert clinicians to the possibility of oropharyngeal cancer. Because of the changing epidemiology of oropharyngeal cancer, the diagnosis should also be considered in younger (aged 40-60 years) and sexually active people presenting with persistent sore throat, dysphagia, and neck mass. A painless persistent neck mass in an adult requires thorough investigation including imaging and biopsy before a benign diagnosis such as branchial cleft cyst is made. A thorough physical examination of the oropharynx, including any ulceration or tonsillar mass, should be performed. If symptoms persist, refer patients promptly to an ear, nose, and throat surgeon.
Although most primary care physicians lack the necessary equipment for detailed head and neck examination, they play a crucial role in recognising and referring early oropharyngeal cancers, thus and reducing treatment morbidity associated with locoregionally advanced disease.[39]
History
Human papillomavirus (HPV)-associated oropharyngeal cancer classically presents with a painless neck mass. Although most patients with HPV-associated cancer present with nodal disease, this is still considered early stage. Unless discovered incidentally on physical examination or imaging, most HPV-independent oropharyngeal cancers present in advanced stages. Sore throat, oral pain, dysphagia, weight loss, neck mass, and trismus are late symptoms. Dysphagia and weight loss should alert clinicians to the possibility of silent aspiration.[40] The presence or absence of comorbidities should be noted, as they may affect patient management.[41] Elicit a history of tobacco or alcohol use, and quantify tobacco use in pack years.[2]
Physical examination
The general appearance of the patient is important for further management. Evidence of cachexia, malnutrition, trismus, and poor dentition should be noted, as these patients most likely will benefit from prophylactic placement of a gastrostomy tube before treatment.[42] Trismus, inability to protrude the tongue, and presence of a large (>3 cm) and fixed cervical node indicate locally advanced disease.
Use of a head light is important for examining the oropharynx, because it frees both hands for the examination. White (leukoplakia) and red plaques (erythroplakia) should be noted, as they may indicate field cancerisation, distinct from the primary lesion. Ulceration or mass of the soft palate, tonsils, pharyngeal wall, and base of tongue, their size, and their extension to adjacent anatomical sites should be recorded for staging purposes. Use of a local anaesthetic (oral xylocaine or benzocaine spray) is recommended before palpation of the tumour, as it is often painful. Induration of the tumour indicates submucosal spread, which may not be visible. A flexible fibre optic endoscopic examination is strongly recommended to determine tumour extent, as well as to exclude a second primary in the larynx and hypopharynx. However, in experienced hands, a mirror examination of these sites can provide adequate information for patient management.
Investigations
Imaging
The goal of diagnostic imaging is to establish the location, size, and extent of the tumour. Clinical examination tends to underestimate tumour extent because of its submucosal spread.
The American Joint Committee on Cancer and the National Comprehensive Cancer Network (NCCN) recommend either CT scan or magnetic resonance imaging (MRI) of the head and neck with contrast to evaluate the primary site and any nodal disease.[2][43][44][45]
CT scan is usually the first examination performed because of its short examination time and general availability. Tumour characteristics on CT scan are space-occupying growth with obliteration of fat planes, infiltration of muscles, bony destruction, and peripheral enhancement with intravenous contrast.[Figure caption and citation for the preceding image starts]: Large base of tongue tumour seen on axial CT scanFrom the collection of Dr Linda X. Yin; used with permission [Citation ends].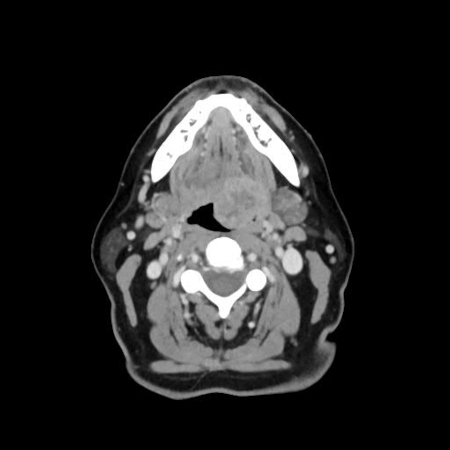
Lymph node enlargement (>1 cm) and central necrosis are indirect signs of malignancy.[44] However, small and superficial tumours may not be seen, and the presence of dental artefacts may obscure the tumour on CT scan.
Tumours have identifiable characteristics on MRI. They usually appear hypointense to muscle on T1-weighted sequence, hyperintense to muscle on T2-weighted sequence, and enhanced with gadolinium contrast. MRI is superior to CT scan in evaluating bone marrow involvement, perineural and prevertebral spread, and pterygopalatine fossa involvement. However, MRI is more susceptible to motion artefact.[45]
PET-CT is indicated if CT or MRI do not reveal an obvious primary tumour.[2] Because most oropharyngeal cancers are locally advanced, PET is particularly useful to detect distant metastases and second primary at cancer diagnosis.[46] Accuracy in detecting distant metastases is 94% with PET-CT, 90% with PET alone, and 74% with CT alone.[47] PET-CT has a high specificity and negative predictive value for the detection of cervical metastatic lymph nodes.[48] PET-CT also improves the accuracy of planning radiotherapy treatment in oropharyngeal cancers that are treated with radiotherapy.[49] PET-CT can be followed by examination under general anaesthesia to complete the staging process if the cancer is advanced.
Biopsy
Patients should be referred to an ear, nose, and throat surgeon for histological diagnosis of either the primary or neck node. The NCCN recommends considering examination under anaesthesia with biopsy confirmation for patients presenting with a p16-positive cervical lymph node prior to treatment decision-making.[2] Patients at high risk for general anaesthesia and those who undergo a thorough examination including tongue base palpation, or those who require systemic therapy/radiotherapy and will not have their treatment plan affected, regardless of surgical evaluation, need not undergo examination under anaesthesia.[2] Base of tongue tumours usually require biopsy under general anaesthesia, while tonsil tumours can be accessed with incisional biopsy in the clinic. If a suspicious neck node has been found, but no primary tumour is detected on examination or imaging, then the next step is fine needle aspiration cytology (FNAC) of the node.[50] This may be guided by ultrasound to improve the accuracy of diagnosis.[51][52] Ultrasound guidance improves the accuracy of fine needle aspiration biopsies in oropharyngeal cancer, compared with palpation guidance. FNAC should be repeated if the initial FNAC is negative.
HPV and p16 testing
To identify HPV status, WHO recommends direct HPV testing (by in situ hybridisation and/or PCR based assays) or indirect testing (by p16 immunohistochemical staining).[1][3][4] The NCCN recommends that all patients with oropharyngeal cancer should undergo tumour HPV testing by p16 immunohistochemistry.[2] When using p16, the 70% cut-off with nuclear and cytoplasmic expression with at least moderate to strong intensity is recommended by NCCN.[2] The College of American Pathologists recommends testing all newly diagnosed patients with oropharyngeal squamous cell carcinoma for high-risk HPV.[53] Determining tumour p16 and HPV status informs prognosis. Of note, in Europe, there can be a high rate of discordance between p16 staining and HPV in situ hybridisation results, suggesting there may be value in using both tests on the pathological specimen.
Triple endoscopy
A triple endoscopy (nasolaryngopharyngoscopy, oesophagoscopy, and bronchoscopy), also known as a panendoscopy, can also be performed to exclude a second primary, which is present in approximately 4% of patients.[54][55] There is debate about the benefit of performing triple endoscopy in the era of the positron emission tomography (PET) scan.[56] However, current PET scanners cannot detect lesions smaller than 7 mm in diameter.[57] Given the potential benefit of triple endoscopy in early detection of small second primary lesions in people at higher risk, triple endoscopy can be seen as complementary to PET scanning in selected patients, particularly if the patient has risk factors such as smoking and heavy alcohol use.[Figure caption and citation for the preceding image starts]: 74-year-old man with squamous cell carcinoma of the left tongue base extending into the hypopharynx. Fluorodeoxyglucose PET/CT images demonstrate focal increased metabolic activity in the left hypopharynx/tongue base (arrows)From the collection of Dr Fabio Almeida; used with permission [Citation ends].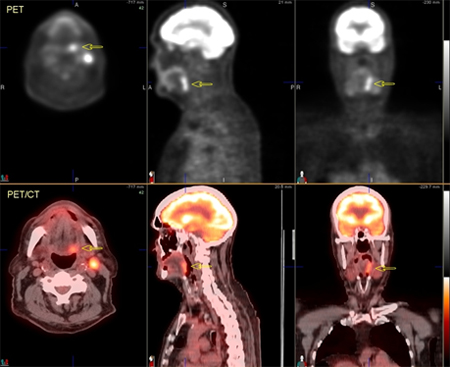 [Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. Fluorodeoxyglucose PET/CT images demonstrate focal increased metabolic activity in the right tongue base, which extends inferior to the hypopharynx (arrows) and across the midline. On the CT images (top row), soft-tissue irregularity can be seen, but the margins of the tumour are difficult to defineFrom the collection of Dr Fabio Almeida; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. Fluorodeoxyglucose PET/CT images demonstrate focal increased metabolic activity in the right tongue base, which extends inferior to the hypopharynx (arrows) and across the midline. On the CT images (top row), soft-tissue irregularity can be seen, but the margins of the tumour are difficult to defineFrom the collection of Dr Fabio Almeida; used with permission [Citation ends].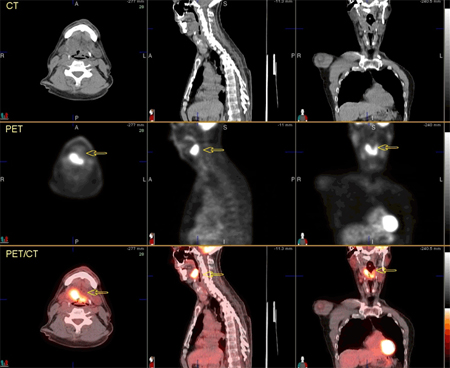 [Figure caption and citation for the preceding image starts]: 74-year-old man with squamous cell carcinoma of the left tongue base extending into the hypopharynx. Images after chemoradiotherapy, showing complete resolution of metabolic foci. Mild diffuse increased metabolism in the oropharyngeal region consistent with mild post-therapy inflammationFrom the collection of Dr Fabio Almeida; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: 74-year-old man with squamous cell carcinoma of the left tongue base extending into the hypopharynx. Images after chemoradiotherapy, showing complete resolution of metabolic foci. Mild diffuse increased metabolism in the oropharyngeal region consistent with mild post-therapy inflammationFrom the collection of Dr Fabio Almeida; used with permission [Citation ends].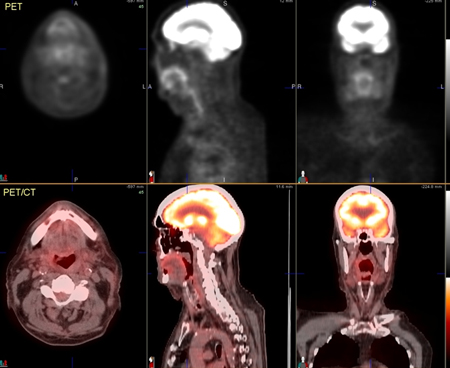 [Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. PET/CT images show mild increased metabolism in a mid right neck lymph node, of concern for metastatic involvement (arrows)From the collection of Dr Fabio Almeida; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. PET/CT images show mild increased metabolism in a mid right neck lymph node, of concern for metastatic involvement (arrows)From the collection of Dr Fabio Almeida; used with permission [Citation ends].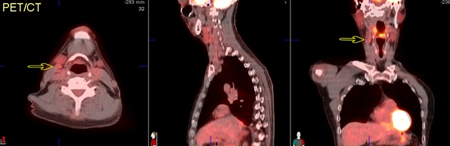 [Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. Axial images further caudally show extent of tumour involvement in the hypopharynx, including invasion through the hyoid boneFrom the collection of Dr Fabio Almeida; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: 60-year-old man with squamous cell carcinoma of the right tongue base. Axial images further caudally show extent of tumour involvement in the hypopharynx, including invasion through the hyoid boneFrom the collection of Dr Fabio Almeida; used with permission [Citation ends].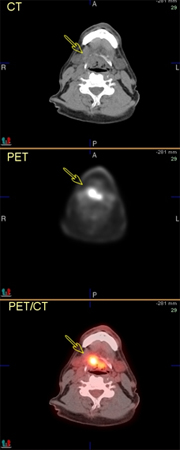
Ancillary studies
A modified barium swallow should be performed if the patient has locally advanced stage cancer or weight loss, to exclude silent aspiration.[40] A percutaneous gastrostomy tube should be inserted in case of aspiration to prevent development of aspiration pneumonia. Patients with compromised nutrition should be considered for tube feedings. Full blood count, chemical profile, albumin, and pre-albumin should be measured to assess the patient's nutritional status before treatment, because of the expected mucositis with radiotherapy or dysphagia after surgery.
Use of this content is subject to our disclaimer