Investigations
1st investigations to order
flexible nasolaryngoscopy
Test
Flexible nasolaryngoscopy is the standard assessment of paradoxical vocal fold motion (intermittent laryngeal obstruction) (PVFM/ILO) during continuous exercise and/or exposure to irritant stimuli.[6][20][31][39][54][74] Continuous laryngoscopy during exercise is a standard assessment for patients with exercise-induced PVFM/ILO.[54][77] It allows full visualisation of the larynx during resting breathing, talking, and swallowing.[Figure caption and citation for the preceding image starts]: Normal larynx: normal colour of vocal folds and surrounding structures, smooth vocal fold edgesFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].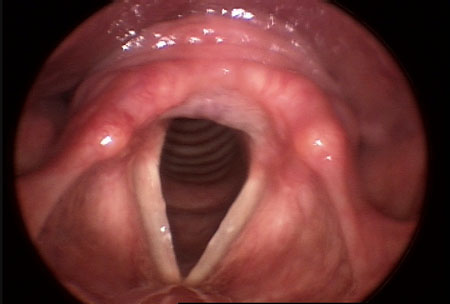
The larynx can also be visualised while the patient reproduces the breathing attack and/or noisy breathing.[Figure caption and citation for the preceding image starts]: Reproduction of breathing attack: adduction of arytenoid complex during inhalationFrom the collection of the University of Wisconsin School of Medicine and Public Health [Citation ends].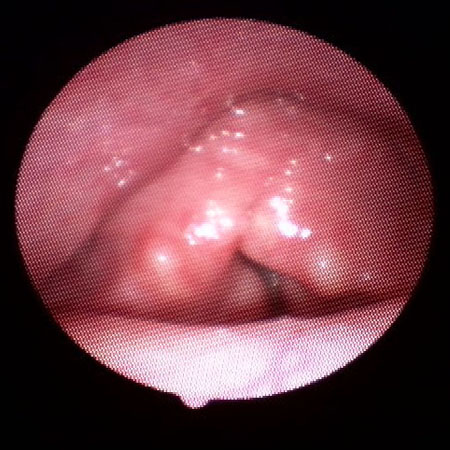
Identification of adduction during inspiration or early expiration can be observed during an asymptomatic state, during symptoms, or with a provocative study to support a diagnosis of PVFM/ILO.[39] However, the classic signs of vocal fold adduction may not always appear on exercise laryngoscopy. In a study with 23 patients the glottic opening ranged from 70% to 86% open during exercise.[77]
Allows exclusion of other aetiologies including upper-airway obstruction, space-occupying lesions, laryngomalacia, laryngeal tremor, vocal fold paresis/paralysis, and post-intubation phonatory insufficiency.[76]
Performed by an experienced speech language pathologist or specialised otolaryngologist.
Result
signs of laryngeal reflux: 1 or more of sub-glottic, vocal fold, or diffuse laryngeal oedema, erythema/hyperaemia, posterior commissure hypertrophy, granuloma/granulation, thick endolaryngeal mucus; arytenoid movement (indicative of PVFM/ILO) during resting breathing; laryngeal narrowing during adduction on reproduction of breathing attack
PFTs/flow-volume plot
Test
Assessment can be performed through spirometry and/or exercise bronchoprovocation. Testing can help to differentiate between restrictive and obstructive airway disorders.
Spirometry will yield diagnostic results, but the patient may require more advanced exercise assessment in the pulmonary laboratory. Variable extrathoracic airway obstruction (truncated inspiratory flow volume loop) may suggest vocal cord dysfunction.[75][81]
Result
truncated inspiratory loop on flow volume plot, normal total lung capacity, comorbid asthma, other pulmonary obstructive or restrictive disorders, low forced vital capacity, low forced inspiratory vital capacity, and low forced inspiratory volume at 0.5 seconds of the inspiratory phase
Investigations to consider
sinus CT
Test
Undertaken in order to rule out chronic sinus disease in patients with nasal complaints.[79]
Result
minimum or absence of sinus inflammation
laryngeal sensory discrimination testing
Test
Air pulse stimulus delivered to the laryngeal mucosa (innervated by the superior laryngeal nerve) via a flexible fibre-optic nasendoscopy in order to determine its level of sensitivity.[80]
Patients with paradoxical vocal fold motion (intermittent laryngeal obstruction) and laryngopharyngeal reflux (LPR), as well as those with GORD and cough, have decreased laryngeal sensitivity as assessed with laryngeal sensory discrimination testing.[38][50]
Most commonly used for assessment of swallowing disorders and risk of aspiration.
Not routinely done in all centres, and there is ongoing research into its effectiveness.
Result
laryngeal sensitivity threshold (normal <4.0 mmHg, moderate deficit 4.0-6.0 mmHg, severe deficit >6.0 mmHg)
Use of this content is subject to our disclaimer