Aetiology
Causes may be ophthalmological (with corneal disease the most common), vascular, neurological, oncological, or diabetic.
Other common causes are usually chronic and include cataract and diabetic retinopathy.
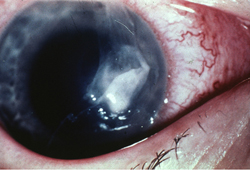
Acute causes are less common and include retinal vascular occlusion, retinal inflammation, retinal infection, optic neuritis, and ischaemic optic neuropathy. [Figure caption and citation for the preceding image starts]: Corneal ulcer with epithelial defect and stromal infiltrateFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].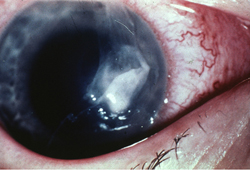 [Figure caption and citation for the preceding image starts]: Central retinal vein occlusion: extensive retinal haemorrhages and dilated vesselsFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
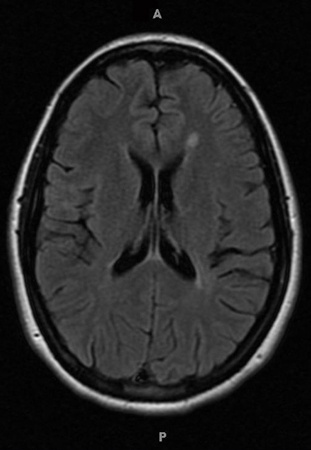
[Figure caption and citation for the preceding image starts]: Central retinal vein occlusion: extensive retinal haemorrhages and dilated vesselsFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Typical white matter lesions indicative of multiple sclerosis risk (MRI)From Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Typical white matter lesions indicative of multiple sclerosis risk (MRI)From Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].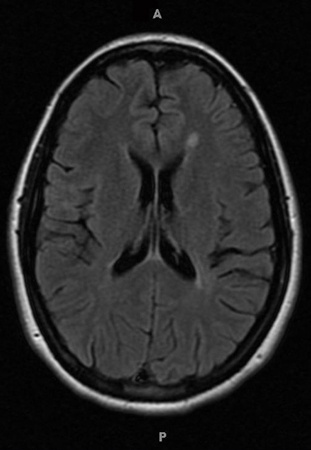 [Figure caption and citation for the preceding image starts]: Segmental optic disc swelling and haemorrhage seen in non-arteritic ischaemic optic neuropathyFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Segmental optic disc swelling and haemorrhage seen in non-arteritic ischaemic optic neuropathyFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].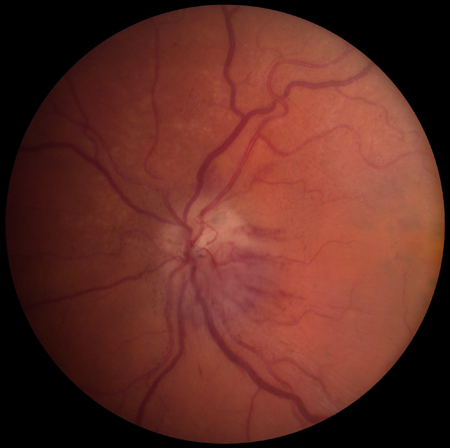
Corneal
Often represents acute exacerbations of chronic disorders. Includes corneal hydrops, dry eye (also known as tear dysfunction syndrome), and keratoconus. There is often a history of corneal disease and/or contact lens wear.
Consider corneal ulcer in all contact lens wearers who present acutely with eye pain/redness. In these patients, prompt treatment is essential to avoid permanent vision loss.[12][Figure caption and citation for the preceding image starts]: Corneal ulcer with epithelial defect and stromal infiltrateFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
Optic nerve disorders
Optic neuritis is most commonly caused by demyelination, and typically develops in females of childbearing age.[13] Central vision, peripheral vision, or both may be decreased sub-acutely. The condition is often associated with pain, particularly on eye movement. Visual field loss tends to respect anatomical (horizontal) boundaries. Significant proportions of people with multiple sclerosis (MS) develop optic neuritis or present with symptoms of optic neuritis. Optic nerve lesions due to MS resemble cerebral lesions found in people with MS.
Papilloedema is optic disc swelling secondary to raised intracranial pressure. Causes include ventricular obstruction, cerebral oedema, intracranial hypertension, and poor cerebrospinal fluid absorption.
Leber's hereditary optic neuropathy is a maternally inherited mitochondrial mutation that commonly affects young men.
Infectious causes of optic nerve dysfunction are uncommon but include tuberculosis, syphilis, borreliosis, hepatitis B, herpes, and cytomegalovirus.
Treatment-induced causes of optic nerve dysfunction can occur secondary to medications (such as etanercept, isoniazid, ethambutol, interferon alfa), and radiotherapy.[Figure caption and citation for the preceding image starts]: Typical white matter lesions indicative of multiple sclerosis risk (MRI)From Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
Glaucoma
Acute glaucoma occurs when there is a rapid marked increase in intraocular pressure (IOP), and may lead to sudden vision loss.[14][15]
Acute angle-closure glaucoma typically presents with a painful red eye in the setting of increased IOP. Gastrointestinal symptoms such as nausea and vomiting may also occur.[16]
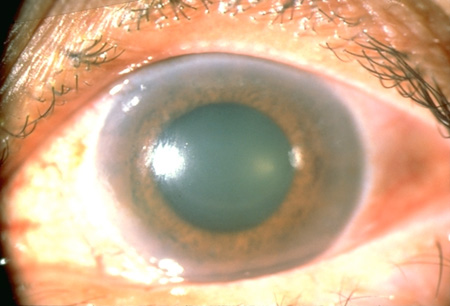
Patients with a history of severe diabetic retinopathy or retinal vascular disease are at risk for neovascular glaucoma, characterised by new blood vessel growth in the anterior chamber angle secondary to ocular ischaemia.[Figure caption and citation for the preceding image starts]: Angle-closure glaucoma: the pupil is mid-dilated, and the cornea is oedematous and cloudy, as indicated by the dulled and irregular light reflexFrom Dr Prem S. Subramanian's personal collection, used with permission [Citation ends].
Retinal
Patient age is important when assessing for retinal disease.
Patients >50 years of age presenting with sudden painless central vision loss often have age-related macular degeneration (AMD). Dry AMD results from the build-up of drusen in the retinal pigment epithelium (RPE), eventually causing loss of RPE with resulting vision loss. Wet AMD results from choroidal neovascularisation and subsequent bleeding beneath, and within, the retina. Vision loss from AMD is typically slow and chronic, but may present acutely.[17]
Males with moderate to high myopia are at greatest risk for retinal detachment. This risk is increased after cataract surgery.[4] Presentation may be acute, with the onset of monocular floaters or flashes.[18] These symptoms may progress to gradual loss of vision (often described as a 'curtain' moving across vision in one eye) and, if untreated, to total vision loss.
Retinal vascular occlusion may produce similar symptoms to retinal detachment.[19][20]
Diabetic and oncological retinopathies also occur.[Figure caption and citation for the preceding image starts]: Central retinal vein occlusion: extensive retinal haemorrhages and dilated vesselsFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].

Inflammatory
Patients with autoimmune diseases (such as rheumatoid arthritis, lupus, or ulcerative colitis) may experience loss of vision due to anterior or posterior uveitis, retinal vasculitis, or optic neuritis.
Vision loss may occur at any time in the course of the disease and may be the presenting symptom.
Pain usually results from ciliary muscle spasm secondary to intraocular inflammation.
Patients with panuveitis and posterior uveitis often have vitreous opacity, retinal oedema, retinal haemorrhage, lipid deposition, and/or optic nerve involvement.[21]
Patients with anterior uveitis often have photophobia and a red eye with minimal vision changes.
Ophthalmological evaluation is essential to diagnose ocular inflammatory disease.
Lens disorders
Deterioration of vision is usually slow and painless, although it can also occur rapidly.
Patients may present acutely upon discovering poor vision when covering or closing the unaffected eye. Cataract rarely requires urgent referral.
The question of screening of the older population, particularly to prevent road traffic accidents, is widely debated.[22] In 2022, the US Preventive Services Task Force concluded that the current evidence is insufficient to assess the balance of benefits and harms of screening for impaired visual acuity in older adults.[23]
Myopic lens shift can occur in people with or without diabetes and results in decreased visual acuity, although this can typically be improved with corrective lenses.
Ophthalmovascular
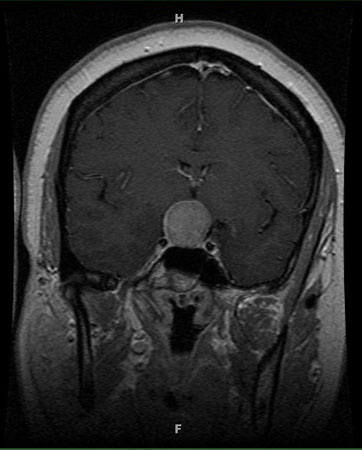
The vascular processes involved in pituitary apoplexy usually develop acutely as extensions of existing pituitary adenomas. Neurological impairment typically results.
Retinal venous or arterial occlusion causes acute monocular vision loss due to atherosclerosis. Symptoms are similar to those of retinal detachment. The risk factors for retinal vascular disease are similar to those that result in systemic vascular disease.[24][25][26] Although rare, retinal artery occlusion can occur due to periocular injections of aesthetic treatments and fillers.[27]
Amaurosis fugax is transient, painless, monocular vision loss most commonly due to carotid artery atheroma or cardiac embolus passage into the central retinal artery.[28] Amaurosis fugax may also occur in a patient with giant cell arteritis.[29]
Vitreous haemorrhage can be caused by retinal tears or neovascularisation. It produces acute, monocular, and usually painless symptoms.
Ischaemic optic neuropathy is most common over the age of 50 years and often presents acutely.[30] Anterior ischaemic optic neuropathy can be arteritic due to giant cell arteritis, or non-arteritic. Giant cell arteritis commonly affects the posterior ciliary arteries and ophthalmic arteries, causing sudden vision loss.
Wet AMD may result from choroidal neovascularisation in older patients.[17][31][Figure caption and citation for the preceding image starts]: Central retinal vein occlusion: extensive retinal haemorrhages and dilated vesselsFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Pituitary apoplexy: large suprasellar mass with heterogeneous gadolinium enhancement (T1-weighted MRI)From Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Pituitary apoplexy: large suprasellar mass with heterogeneous gadolinium enhancement (T1-weighted MRI)From Dr Prem S. Subramanian's personal collection; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Pituitary tumour: homogenous suprasellar mass elevating and compressing optic chiasm (MRI)From Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Pituitary tumour: homogenous suprasellar mass elevating and compressing optic chiasm (MRI)From Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].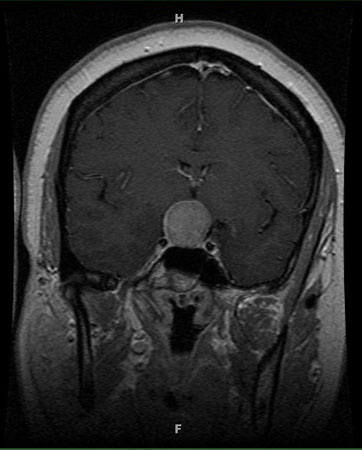 [Figure caption and citation for the preceding image starts]: Sub-retinal haemorrhage and retinal elevation from sub-foveal neovascularisationFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Sub-retinal haemorrhage and retinal elevation from sub-foveal neovascularisationFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Fluorescein angiogram showing classic choroidal neovascularisation with early hyperfluorescenceFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Fluorescein angiogram showing classic choroidal neovascularisation with early hyperfluorescenceFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].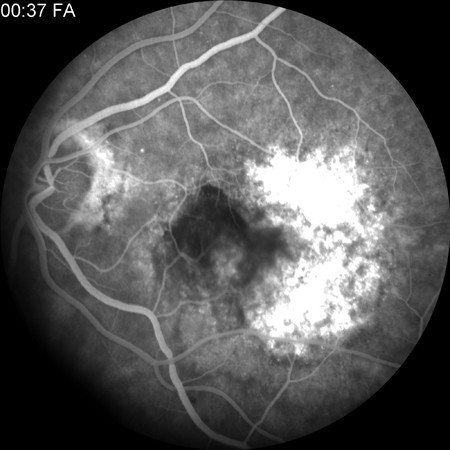
Neurovascular
Atherosclerosis can cause amaurosis fugax, transient ischaemic attack, and ischaemic stroke.
Haemorrhagic or ischaemic stroke can cause homonymous hemianopia or central vision loss. The resultant visual defect is usually determined by the site of ischaemia or haemorrhage.
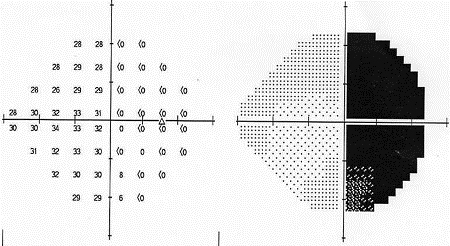
Migraine headache or migraine aura without headache (acephalgic migraine) can be associated with transient loss or impairment of vision.[Figure caption and citation for the preceding image starts]: Right eye of patient with homonymous field defectFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Left eye of patient with homonymous field defectFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Left eye of patient with homonymous field defectFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].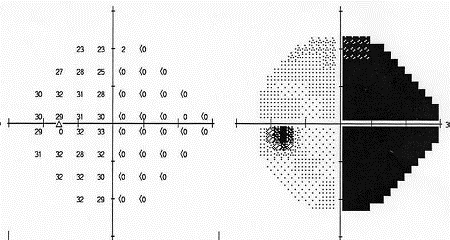
Oncological
Cancer-associated retinopathy is rare but severe and rapidly progressive. It is a paraneoplastic disorder characterised by antibodies to the photoreceptor protein recoverin, and is usually associated with small cell lung cancer. Similar entities include melanoma-associated retinopathy and paraneoplastic optic neuropathy.
Cerebral tumours can cause homonymous hemianopia. The resultant visual defect is determined by lesion site.
Pituitary tumours commonly cause vision loss. These patients require endocrine and neurosurgical consultations.
[Figure caption and citation for the preceding image starts]: Pituitary tumour: homogenous suprasellar mass elevating and compressing optic chiasm (MRI)From Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
 [Figure caption and citation for the preceding image starts]: Right eye of patient with homonymous field defectFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Right eye of patient with homonymous field defectFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].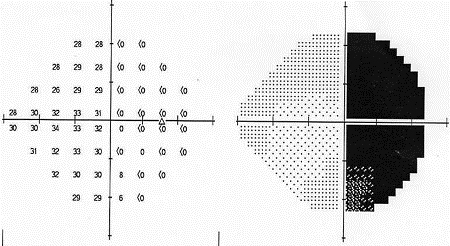 [Figure caption and citation for the preceding image starts]: Left eye of patient with homonymous field defectFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Left eye of patient with homonymous field defectFrom Dr Prem S. Subramanian's personal collection; used with permission [Citation ends].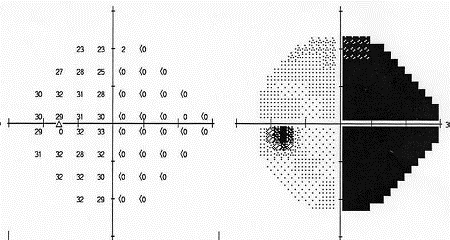
Diabetic
Diabetic retinopathies may develop before systemic diabetes is diagnosed.
Pathophysiology is unproved; however, severity and speed to progression is closely linked to diabetic control. Contributing factors may include growth hormone, platelets, blood viscosity, aldose reductase, and vasoproliferation.
Consider measuring blood glucose levels in all patients presenting with vision loss. Arrange an ophthalmology examination for all patients with newly diagnosed diabetes.[9][10]
Vision loss in people with diabetes can also be due to cataracts, myopic lens shift, glaucoma, neuropathies, and other corneal abnormalities.
Traumatic
Closed head injury may cause traumatical optic neuropathy and acute vision loss.
Injury to the occipital poles may cause bilateral central vision loss due to occipital lobe contusion.
Head injury (open or closed) can cause homonymous hemianopia. The resultant visual defect is determined by anatomic site of injury.
Globe injury may lead to vision loss from frank globe rupture or penetration by foreign bodies. Closed globe trauma may cause hyphaema, lens dislocation, vitreous haemorrhage, retinal contusion (commotio retinae or Berlin's oedema), and retinal detachment.
Severe orbital trauma may cause increased orbital pressure and retinal vascular occlusion. Orbital haemorrhage results in rapidly progressive vision loss from compressive optic neuropathy.
Rarely, Terson's syndrome causes vision loss. It occurs when there is any intra-ocular haemorrhage, including vitreous, sub-hyaloid, intraretinal, or sub-retinal bleeding, in patients with intracranial haemorrhage or traumatic brain injury.
Use of this content is subject to our disclaimer