Most people with Meckel's diverticulum are asymptomatic. The diagnosis of Meckel's diverticulum is frequently an incidental finding during an imaging study or operative exploration.[3]Yahchouchy EK, Marano AF, Etienne JC, et al. Meckel's diverticulum. J Am Coll Surg. 2001 May;192(5):658-62.
http://www.ncbi.nlm.nih.gov/pubmed/11333103?tool=bestpractice.com
[13]Turgeon DK, Barnett JL. Meckel's diverticulum. Am J Gastroenterol. 1990;85:777-81.[18]Gan T, Evers MB. Meckel diverticulum. In: Townsend CM Jr. Sabiston textbook of surgery. 21st ed. St. Louis, MO: Elsevier; 2021:1240-300.[22]Matsagas MI, Fatouros M, Koulouras B, et al. Incidence, complications, and management of Meckel's diverticulum. Arch Surg. 1995;130:143-146.
http://www.ncbi.nlm.nih.gov/pubmed/7848082?tool=bestpractice.com
[23]Martin JP, Connor PD, Charles K. Meckel's diverticulum. Am Fam Physician. 2000;61:1037-1042,1044.
http://www.aafp.org/afp/2000/0215/p1037.html
http://www.ncbi.nlm.nih.gov/pubmed/10706156?tool=bestpractice.com
Physical examination and laboratory evaluation are usually normal in asymptomatic patients.
Risk factors for the development of symptoms include male sex and age <2 years.
Consider Meckel's diverticulum as a possible diagnosis in patients with symptoms of gastrointestinal (GI) bleeding, intestinal obstruction, peritonitis, and/or perforation.[3]Yahchouchy EK, Marano AF, Etienne JC, et al. Meckel's diverticulum. J Am Coll Surg. 2001 May;192(5):658-62.
http://www.ncbi.nlm.nih.gov/pubmed/11333103?tool=bestpractice.com
[13]Turgeon DK, Barnett JL. Meckel's diverticulum. Am J Gastroenterol. 1990;85:777-81.[23]Martin JP, Connor PD, Charles K. Meckel's diverticulum. Am Fam Physician. 2000;61:1037-1042,1044.
http://www.aafp.org/afp/2000/0215/p1037.html
http://www.ncbi.nlm.nih.gov/pubmed/10706156?tool=bestpractice.com
[24]Cullen JJ, Kelly KA, Moir CR, et al. Surgical management of Meckel's diverticulum: an epidemiologic, population-based study. Ann Surg. 1994 Oct;220(4):564-8; discussion 568-9.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1234434/pdf/annsurg00056-0170.pdf
http://www.ncbi.nlm.nih.gov/pubmed/7944666?tool=bestpractice.com
Rule of 2s
A useful mnemonic describing Meckel's diverticulum is the 'rule of 2s': 2% prevalence; 2:1 male:female ratio for symptomatic presentations; location most commonly 2 feet (60 cm) proximal to ileocaecal valve in adults; 2 types of ectopic tissue (gastric and pancreatic); commonly 2 inches (5 cm) long; and half of those symptomatic are younger than 2 years of age.[25]Tavakkoli A, Ashley SW, Zinner MJ. Small intestine. In: Brunicardi FC, Andersen DK, Billiar TR, et al, eds. Schwartz's principles of surgery. 10th ed. New York, NY: McGraw-Hill; 2015.
Clinical evaluation of symptomatic patients
Bleeding
GI bleeding is a common presenting symptom in both children and adults (30% to 40% of cases).[1]Hansen CC, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel's diverticulum in the 21st century. Medicine (Baltimore). 2018 Aug;97(35):e12154.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6392637
http://www.ncbi.nlm.nih.gov/pubmed/30170459?tool=bestpractice.com
[3]Yahchouchy EK, Marano AF, Etienne JC, et al. Meckel's diverticulum. J Am Coll Surg. 2001 May;192(5):658-62.
http://www.ncbi.nlm.nih.gov/pubmed/11333103?tool=bestpractice.com
[14]Sagar J, Kumar V, Shah DK. Meckel's diverticulum: a systematic review. J R Soc Med. 2006;99:501-5.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1592061
http://www.ncbi.nlm.nih.gov/pubmed/17021300?tool=bestpractice.com
[15]St-Vil D, Brandt ML, Panic S, et al. Meckel’s diverticulum in children: a 20-year review. J Pediatr Surg. 1991:26:1289-1292.
http://www.ncbi.nlm.nih.gov/pubmed/1812259?tool=bestpractice.com
Up to 90% of bleeding diverticula contain heterotopic gastric mucosa that secretes acid, resulting in ileal mucosal ulceration adjacent to the diverticulum.[13]Turgeon DK, Barnett JL. Meckel's diverticulum. Am J Gastroenterol. 1990;85:777-81.
Classically, the bleeding is acute, episodic, and painless.
Patients may also be haemodynamically unstable, with tachycardia and hypotension.
Obstruction
Small bowel obstruction is one of the commonest presentations in both children and adults, accounting for 40% to 50% of symptomatic cases.[1]Hansen CC, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel's diverticulum in the 21st century. Medicine (Baltimore). 2018 Aug;97(35):e12154.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6392637
http://www.ncbi.nlm.nih.gov/pubmed/30170459?tool=bestpractice.com
[3]Yahchouchy EK, Marano AF, Etienne JC, et al. Meckel's diverticulum. J Am Coll Surg. 2001 May;192(5):658-62.
http://www.ncbi.nlm.nih.gov/pubmed/11333103?tool=bestpractice.com
[15]St-Vil D, Brandt ML, Panic S, et al. Meckel’s diverticulum in children: a 20-year review. J Pediatr Surg. 1991:26:1289-1292.
http://www.ncbi.nlm.nih.gov/pubmed/1812259?tool=bestpractice.com
Patients present with intractable constipation (obstipation), crampy abdominal pain, nausea, and vomiting.
A palpable abdominal mass may, rarely, be present, if intussusception is the cause of the obstruction.[18]Gan T, Evers MB. Meckel diverticulum. In: Townsend CM Jr. Sabiston textbook of surgery. 21st ed. St. Louis, MO: Elsevier; 2021:1240-300. Patients with intussusception may also have dark red, maroon, or 'currant jam' stools.
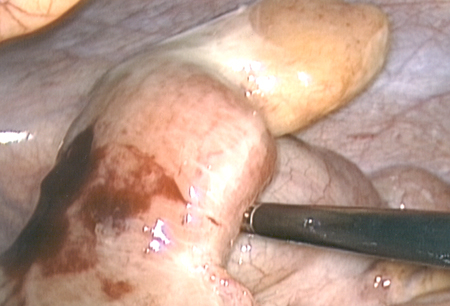
Inflammation and perforation
Meckel's diverticulitis is usually seen in adults rather than children, and accounts for 20% to 35% of symptomatic cases in adults.[18]Gan T, Evers MB. Meckel diverticulum. In: Townsend CM Jr. Sabiston textbook of surgery. 21st ed. St. Louis, MO: Elsevier; 2021:1240-300.[19]Parvanescu A, Bruzzi M, Voron T, et al. Complicated Meckel's diverticulum: presentation modes in adults. Medicine (Baltimore). 2018 Sep;97(38):e12457.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6160168
http://www.ncbi.nlm.nih.gov/pubmed/30235734?tool=bestpractice.com
[Figure caption and citation for the preceding image starts]: Inflamed Meckel's diverticulumFrom the collection of Dr Ali Tavakkoli; used with permission [Citation ends].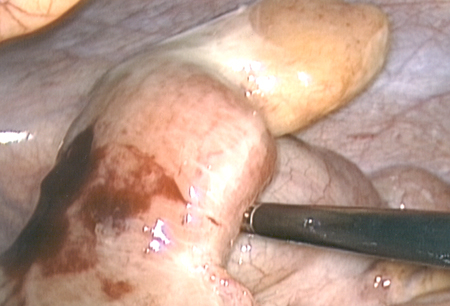
Clinical presentation is typically abdominal pain in the periumbilical area that radiates to the right lower quadrant.[3]Yahchouchy EK, Marano AF, Etienne JC, et al. Meckel's diverticulum. J Am Coll Surg. 2001 May;192(5):658-62.
http://www.ncbi.nlm.nih.gov/pubmed/11333103?tool=bestpractice.com
It is often clinically indistinguishable from acute appendicitis and may be diagnosed during preoperative imaging or during surgical exploration.[3]Yahchouchy EK, Marano AF, Etienne JC, et al. Meckel's diverticulum. J Am Coll Surg. 2001 May;192(5):658-62.
http://www.ncbi.nlm.nih.gov/pubmed/11333103?tool=bestpractice.com
[13]Turgeon DK, Barnett JL. Meckel's diverticulum. Am J Gastroenterol. 1990;85:777-81.[19]Parvanescu A, Bruzzi M, Voron T, et al. Complicated Meckel's diverticulum: presentation modes in adults. Medicine (Baltimore). 2018 Sep;97(38):e12457.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6160168
http://www.ncbi.nlm.nih.gov/pubmed/30235734?tool=bestpractice.com
[26]Cullen JJ, Kelly KA. Current management of Meckel's diverticulum. Adv Surg. 1996;29:207-14.
http://www.ncbi.nlm.nih.gov/pubmed/8720004?tool=bestpractice.com
In general, a Meckel's diverticulum is less prone to inflammation than the appendix, because most diverticula have a wide mouth and are therefore less likely to become obstructed.
Diverticular obstruction can lead to distal inflammation, necrosis, and perforation, resulting in an abscess, peritonitis, or, rarely, haemoperitoneum.[6]Burt BM, Tavakkolizadeh A, Ferzoco SJ. Meckel's hemoperitoneum: a rare case of Meckel's diverticulitis causing intraperitoneal hemorrhage. Dig Dis Sci. 2006;51:1546-1548.
http://www.ncbi.nlm.nih.gov/pubmed/16927155?tool=bestpractice.com
Meckel's diverticulitis or small bowel obstruction may progress to bowel perforation. If perforation is present, patients may present with a diffuse abdominal tenderness.
Investigation of symptomatic patients
Bleeding
All patients require an FBC, which may show a significantly decreased haemoglobin and haematocrit. Leukocytosis with a left shift may be present.
In haemodynamically stable patients with occult bleeding, capsule endoscopy is often used as part of the work-up, and may provide direct observation of Meckel's diverticulum in adults and children.[27]Sengupta N, Kastenberg DM, Bruining DH, et al. The role of imaging for GI bleeding: ACG and SAR consensus recommendations. Radiology. 2024 Mar;310(3):e232298.
https://pubs.rsna.org/doi/10.1148/radiol.232298
http://www.ncbi.nlm.nih.gov/pubmed/38441091?tool=bestpractice.com
[28]Krstic SN, Martinov JB, Sokic-Milutinovic AD, et al. Capsule endoscopy is useful diagnostic tool for diagnosing Meckel's diverticulum. Eur J Gastroenterol Hepatol. 2016 Jun;28(6):702-7.
http://www.ncbi.nlm.nih.gov/pubmed/26854797?tool=bestpractice.com
[29]Li L, Zhan X, Chen Y, et al. Application of small bowel capsule endoscopy in children with Meckel's diverticulum. Eur J Gastroenterol Hepatol. 2024 Jul 1;36(7):845-9.
https://pmc.ncbi.nlm.nih.gov/articles/PMC11288385
http://www.ncbi.nlm.nih.gov/pubmed/38829942?tool=bestpractice.com
[30]Baltes P, Dray X, Riccioni ME, et al. Small-bowel capsule endoscopy in patients with Meckel's diverticulum: clinical features, diagnostic workup, and findings. A European multicenter I-CARE study. Gastrointest Endosc. 2023 May;97(5):917-26.e3.
http://www.ncbi.nlm.nih.gov/pubmed/36572128?tool=bestpractice.com
Guidelines on imaging for gastrointestinal bleeding recommend cross-sectional imaging with CT enterography if capsule endoscopy is negative or contraindicated.[27]Sengupta N, Kastenberg DM, Bruining DH, et al. The role of imaging for GI bleeding: ACG and SAR consensus recommendations. Radiology. 2024 Mar;310(3):e232298.
https://pubs.rsna.org/doi/10.1148/radiol.232298
http://www.ncbi.nlm.nih.gov/pubmed/38441091?tool=bestpractice.com
However, an uncomplicated Meckel's diverticulum may be difficult to visualise with CT enterography.[27]Sengupta N, Kastenberg DM, Bruining DH, et al. The role of imaging for GI bleeding: ACG and SAR consensus recommendations. Radiology. 2024 Mar;310(3):e232298.
https://pubs.rsna.org/doi/10.1148/radiol.232298
http://www.ncbi.nlm.nih.gov/pubmed/38441091?tool=bestpractice.com
For patients with suspected Meckel's diverticulum without active bleeding, request a technetium-99m pertechnetate scan ('Meckel's scan').[31]Spottswood SE, Pfluger T, Bartold SP, et al. SNMMI and EANM practice guideline for meckel diverticulum scintigraphy 2.0. J Nucl Med Technol. 2014 Sep;42(3):163-9.
https://tech.snmjournals.org/content/42/3/163.long
http://www.ncbi.nlm.nih.gov/pubmed/24948825?tool=bestpractice.com
A Meckel's scan is considered the imaging modality of choice for diagnosis of Meckel's diverticulum in children, but a negative result does not exclude the possibility. This scan takes advantage of the way the tracer accumulates in certain tissues, including ectopic gastric tissue that is sometimes found in Meckel's diverticulum. Studies show a sensitivity of 0.80 (95% CI: 0.73 to 0.86) and specificity of 0.95 (95% CI: 0.86 to 0.98), with lower sensitivity in adults.[32]Yan P, Jiang S. Tc-99m scan for pediatric bleeding Meckel diverticulum: a systematic review and meta-analysis. J Pediatr (Rio J). 2023 Sep-Oct;99(5):425-31.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10492155
http://www.ncbi.nlm.nih.gov/pubmed/37277097?tool=bestpractice.com
[33]Lindeman RJ, Søreide K. The many faces of Meckel's Diverticulum: update on management in incidental and symptomatic patients. Curr Gastroenterol Rep. 2020 Jan 13;22(1):3.
http://www.ncbi.nlm.nih.gov/pubmed/31930430?tool=bestpractice.com
In patients with active bleeding or hemodynamic instability, CT angiography or mesenteric angiography is the preferred initial investigation.[27]Sengupta N, Kastenberg DM, Bruining DH, et al. The role of imaging for GI bleeding: ACG and SAR consensus recommendations. Radiology. 2024 Mar;310(3):e232298.
https://pubs.rsna.org/doi/10.1148/radiol.232298
http://www.ncbi.nlm.nih.gov/pubmed/38441091?tool=bestpractice.com
[33]Lindeman RJ, Søreide K. The many faces of Meckel's Diverticulum: update on management in incidental and symptomatic patients. Curr Gastroenterol Rep. 2020 Jan 13;22(1):3.
http://www.ncbi.nlm.nih.gov/pubmed/31930430?tool=bestpractice.com
Active bleeding can cause false negatives on Meckel's scan.[33]Lindeman RJ, Søreide K. The many faces of Meckel's Diverticulum: update on management in incidental and symptomatic patients. Curr Gastroenterol Rep. 2020 Jan 13;22(1):3.
http://www.ncbi.nlm.nih.gov/pubmed/31930430?tool=bestpractice.com
CT angiography is typically performed before conventional angiography as it is faster, non-invasive, and widely accessible.[27]Sengupta N, Kastenberg DM, Bruining DH, et al. The role of imaging for GI bleeding: ACG and SAR consensus recommendations. Radiology. 2024 Mar;310(3):e232298.
https://pubs.rsna.org/doi/10.1148/radiol.232298
http://www.ncbi.nlm.nih.gov/pubmed/38441091?tool=bestpractice.com
Mesenteric angiography can detect haemorrhage in the range of 0.5 to 1.0 mL/min and is generally employed only to localise the bleeding; however, it can have a therapeutic role too.
If primary diagnosis remains unclear or the patient is haemodynamically unstable, a surgical abdominal exploration may be necessary, during which the diagnosis may be established.[18]Gan T, Evers MB. Meckel diverticulum. In: Townsend CM Jr. Sabiston textbook of surgery. 21st ed. St. Louis, MO: Elsevier; 2021:1240-300.[19]Parvanescu A, Bruzzi M, Voron T, et al. Complicated Meckel's diverticulum: presentation modes in adults. Medicine (Baltimore). 2018 Sep;97(38):e12457.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6160168
http://www.ncbi.nlm.nih.gov/pubmed/30235734?tool=bestpractice.com
Obstruction
The initial test for patients with suspected obstruction is a CT scan of the abdomen, which may show the Meckel's diverticulum or related intussusception. Ultrasound may be the preferred option for children.[34]Chatterjee A, Harmath C, Vendrami CL, et al. Reminiscing on remnants: imaging of Meckel diverticulum and its complications in adults. AJR Am J Roentgenol. 2017 Nov;209(5):W287-96.
https://www.ajronline.org/doi/10.2214/AJR.17.18088
http://www.ncbi.nlm.nih.gov/pubmed/28834452?tool=bestpractice.com
[35]Elsayes KM, Menias CO, Harvin HJ, et al. Imaging manifestations of Meckel's diverticulum. AJR Am J Roentgenol. 2007 Jul;189(1):81-8.
https://www.ajronline.org/doi/10.2214/AJR.06.1257
http://www.ncbi.nlm.nih.gov/pubmed/17579156?tool=bestpractice.com
If intussusception is suspected, diagnostic contrast enema may be performed; however, air or hydrostatic reduction in the setting of Meckel's diverticulum has not been found to be useful. Contrast enema is contraindicated if peritonitis, shock, perforation, or an unstable clinical condition is present.[36]American College of Radiology. ACR–SPR practice parameter for the performance of pediatric fluoroscopic contrast enema examinations. 2021 [internet publication].
https://www.acr.org/-/media/ACR/Files/Practice-Parameters/FluourConEnema-Ped.pdf
In cases where intestinal ischaemia or perforation is suspected, and the patient has general peritonitis, an urgent abdominal exploration should be performed without any delays for imaging.
Inflammation
Meckel's diverticulitis is often clinically indistinguishable from appendicitis. A CT scan of the abdomen may show the inflamed Meckel's diverticulum; ultrasound may be preferred in children. However, imaging should not delay surgery if perforation is suspected.[34]Chatterjee A, Harmath C, Vendrami CL, et al. Reminiscing on remnants: imaging of Meckel diverticulum and its complications in adults. AJR Am J Roentgenol. 2017 Nov;209(5):W287-96.
https://www.ajronline.org/doi/10.2214/AJR.17.18088
http://www.ncbi.nlm.nih.gov/pubmed/28834452?tool=bestpractice.com
[35]Elsayes KM, Menias CO, Harvin HJ, et al. Imaging manifestations of Meckel's diverticulum. AJR Am J Roentgenol. 2007 Jul;189(1):81-8.
https://www.ajronline.org/doi/10.2214/AJR.06.1257
http://www.ncbi.nlm.nih.gov/pubmed/17579156?tool=bestpractice.com
Direct observation of Meckel's diverticulum can be helpful in making the diagnosis. This can be done surgically, either by laparoscopy or laparotomy, or with endoscopy of the small intestine.[1]Hansen CC, Søreide K. Systematic review of epidemiology, presentation, and management of Meckel's diverticulum in the 21st century. Medicine (Baltimore). 2018 Aug;97(35):e12154.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6392637
http://www.ncbi.nlm.nih.gov/pubmed/30170459?tool=bestpractice.com
Double-balloon endoscopy allows the endoscope to travel further into the ileum until the Meckel's diverticulum is found and may be considered if other investigations have failed to reveal the diagnosis.
One study comparing capsule endoscopy and double-balloon endoscopy found that double-balloon endoscopy was able to observe 64 of 74 possible Meckel's diverticula.[37]He Q, Zhang YL, Xiao B, et al. Double-balloon enteroscopy for diagnosis of Meckel's diverticulum: comparison with operative findings and capsule endoscopy. Surgery. 2013 Apr;153(4):549-54.
http://www.ncbi.nlm.nih.gov/pubmed/23305600?tool=bestpractice.com
Of the 26 patients who underwent both techniques, 20 of 22 Meckel's diverticula detected by double-balloon endoscopy went undetected on capsule endoscopy. The 10 Meckel's diverticula that were undetected by double-balloon endoscopy were subsequently found on surgery.[37]He Q, Zhang YL, Xiao B, et al. Double-balloon enteroscopy for diagnosis of Meckel's diverticulum: comparison with operative findings and capsule endoscopy. Surgery. 2013 Apr;153(4):549-54.
http://www.ncbi.nlm.nih.gov/pubmed/23305600?tool=bestpractice.com