Obstetric causes can be divided into those in early and late pregnancy. Conditions that span the entire gestation period have been categorised according to their anatomical system. For simplicity, only conditions that more commonly occur ante-partum (before labour commences), rather than intra- or postpartum, have been included.
Early pregnancy
Ectopic pregnancy
Usually diagnosed in the first trimester, most commonly affecting the fallopian tube.[5]Seeber BE, Barnhart KT. Suspected ectopic pregnancy. Obstet Gynecol. 2006 Feb;107(2 Pt 1):399-413.
http://www.ncbi.nlm.nih.gov/pubmed/16449130?tool=bestpractice.com
Strongly associated with conditions that damage the fallopian tube, such as pelvic inflammatory disease (PID), previous ectopic pregnancy, and previous tubal surgery.
Also associated with current IUD users and women whose pregnancy is the result of assisted reproductive technologies.[6]Xiong X, Buekens P, Wollast E. IUD use and the risk of ectopic pregnancy: a meta-analysis of case-control studies. Contraception. 1995 Jul;52(1):23-34.
http://www.ncbi.nlm.nih.gov/pubmed/8521711?tool=bestpractice.com
Ectopic pregnancy incidence following assisted reproductive technology appears to be decreasing with time.[7]Santos-Ribeiro S, Tournaye H, Polyzos NP. Trends in ectopic pregnancy rates following assisted reproductive technologies in the UK: a 12-year nationwide analysis including 160 000 pregnancies. Hum Reprod. 2016 Feb;31(2):393-402.
https://academic.oup.com/humrep/article/31/2/393/2380186
http://www.ncbi.nlm.nih.gov/pubmed/26724796?tool=bestpractice.com
[8]Perkins KM, Boulet SL, Kissin DM, et al. Risk of ectopic pregnancy associated with assisted reproductive technology in the United States, 2001-2011. Obstet Gynecol. 2015 Jan;125(1):70-8.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4315158
http://www.ncbi.nlm.nih.gov/pubmed/25560107?tool=bestpractice.com
Miscarriage
Usually occurs before the 12th week, with approximately 50% of all cases of early pregnancy loss due to fetal chromosomal abnormalities.[9]American College of Obstetricians and Gynecologists' Committee on Practice Bulletins-Gynecology. ACOG practice bulletin no. 200: early pregnancy loss. Obstet Gynecol. 2018 Nov;132(5):e197-207.
https://journals.lww.com/greenjournal/fulltext/2018/11000/acog_practice_bulletin_no__200__early_pregnancy.41.aspx
http://www.ncbi.nlm.nih.gov/pubmed/30157093?tool=bestpractice.com
[10]Stephenson MD, Awartani KA, Robinson WP. Cytogenetic analysis of miscarriages from couples with recurrent miscarriage: a case-control study. Hum Reprod. 2002 Feb;17(2):446-51.
https://academic.oup.com/humrep/article/17/2/446/568974
http://www.ncbi.nlm.nih.gov/pubmed/11821293?tool=bestpractice.com
[11]Menasha J, Levy B, Hirschhorn K, et al. Incidence and spectrum of chromosome abnormalities in spontaneous abortions: new insights from a 12-year study. Genet Med. 2005 Apr;7(4):251-63.
http://www.ncbi.nlm.nih.gov/pubmed/15834243?tool=bestpractice.com
[12]Wu X, Su L, Xie X, et al. Comprehensive analysis of early pregnancy loss based on cytogenetic findings from a tertiary referral center. Mol Cytogenet. 2021 Dec 4;14(1):56.
https://molecularcytogenetics.biomedcentral.com/articles/10.1186/s13039-021-00577-8
http://www.ncbi.nlm.nih.gov/pubmed/34863241?tool=bestpractice.com
Other causes include multiple pregnancy, uterine pathology (e.g., fibroids), cytotoxic drugs, radiation, and systemic conditions (e.g., anti-phospholipid syndrome).
Ovarian hyperstimulation syndrome (OHSS)
At least 2% of pregnancies in industrialised countries are consequent to advanced fertility treatment such as in vitro fertilisation.[13]Human Fertilisation and Embryology. Fertility treatment 2023: trends and figures. Jun 2025 [internet publication].
https://www.hfea.gov.uk/about-us/publications/research-and-data/fertility-treatment-2023-trends-and-figures
Severe OHSS is a potentially life-threatening iatrogenic complication, occurring in approximately 0.5% to 2% of women undergoing gonadotrophin stimulation.[14]Medwin C, Rozen G, Agresta F, et al. The ovarian hyperstimulation that truly matters: admissions, severity and prevention strategies. Aust N Z J Obstet Gynaecol. 2023 Aug;63(4):583-7.
http://www.ncbi.nlm.nih.gov/pubmed/37062907?tool=bestpractice.com
[15]Tomás C, Colmorn L, Rasmussen S, et al. Annual incidence of severe ovarian hyperstimulation syndrome. Dan Med J. 2021 Jan 26;68(2):A12190738.
https://ugeskriftet.dk/dmj/annual-incidence-severe-ovarian-hyperstimulation-syndrome
http://www.ncbi.nlm.nih.gov/pubmed/33543701?tool=bestpractice.com
[16]Courbiere B, Oborski V, Braunstein D, et al. Obstetric outcome of women with in vitro fertilization pregnancies hospitalized for ovarian hyperstimulation syndrome: a case-control study. Fertil Steril. 2011 Apr;95(5):1629-32.
https://www.fertstert.org/article/S0015-0282(10)02957-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/21215968?tool=bestpractice.com
Risk of OHSS is highest in young women with polycystic ovary syndrome or low body mass index.[17]Schirmer DA 3rd, Kulkarni AD, Zhang Y, et al. Ovarian hyperstimulation syndrome after assisted reproductive technologies: trends, predictors, and pregnancy outcomes. Fertil Steril. 2020 Sep;114(3):567-78.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8041489
http://www.ncbi.nlm.nih.gov/pubmed/32680613?tool=bestpractice.com
Severe cases of OHSS are characterised by enlarged ovaries, ascites, increased blood viscosity, and renal or hepatic dysfunction.[18]Al-Shawaf T, Grudzinskas JG. Prevention and treatment of ovarian hyperstimulation syndrome. Best Pract Res Clin Obstet Gynecol. 2003 Apr;17(2):249-61.
http://www.ncbi.nlm.nih.gov/pubmed/12758098?tool=bestpractice.com
Late pregnancy
Pre-term labour
May be triggered by nephrolithiasis, urinary tract infections (UTIs) (particularly pyelonephritis), haemolysis, elevated liver enzymes, low platelet count (HELLP) syndrome, placental abruption (implicated in up to 10% of premature deliveries), chorioamnionitis, and appendicitis.[19]Leitich H. Controversies in diagnosis of preterm labour. BJOG. 2005 Mar;112 Suppl 1:61-3.
http://www.ncbi.nlm.nih.gov/pubmed/15715597?tool=bestpractice.com
Acute cystitis may irritate the uterine segment and trigger uterine contractions.
More likely to occur with non-operative management of cholecystitis compared with those undergoing cholecystectomy.[20]Curet MJ. Special problems in laparoscopic surgery: previous abdominal surgery, obesity, and pregnancy. Surg Clin North Am. 2000 Aug;80(4):1093-110.
http://www.ncbi.nlm.nih.gov/pubmed/10987026?tool=bestpractice.com
Chorioamnionitis
Complicates 1% to 5% of full-term pregnancies and is seen in about 25% of pre-term deliveries.[21]Goldenberg RL. The management of preterm labour. Obstet Gynecol. 2002 Nov;100(5 Pt 1):1020-37.
http://www.ncbi.nlm.nih.gov/pubmed/12423870?tool=bestpractice.com
Associated organisms include Ureaplasma urealyticum, Mycoplasma hominis, Gardnerella vaginalis, Peptostreptococcus, and Bacteroides species.
Risk increased following chorionic villus sampling (CVS) and amniocentesis.
Uterine rupture
High risk in patients who have had previous uterine surgery (e.g., caesarean section, myomectomy).[22]Turner MJ. Uterine rupture. Best Pract Res Clin Obstet Gynaecol. 2002 Feb;16(1):69-79.
http://www.ncbi.nlm.nih.gov/pubmed/11866498?tool=bestpractice.com
Placental abruption
Usually associated with vaginal bleeding.[23]Oyelese Y, Ananth CV. Placental abruption. Obstet Gynecol. 2006 Oct;108(4):1005-16.
https://www.doi.org/10.1097/01.AOG.0000239439.04364.9a
http://www.ncbi.nlm.nih.gov/pubmed/17012465?tool=bestpractice.com
[24]Tikkanen M, Nuutila M, Hiilesmaa V, et al. Clinical presentation and risk factors of placental abruption. Acta Obstet Gynecol Scand. 2006;85(6):700-5.
https://obgyn.onlinelibrary.wiley.com/doi/10.1080/00016340500449915
http://www.ncbi.nlm.nih.gov/pubmed/16752262?tool=bestpractice.com
Risk factors include maternal age ≥35 years, multi-parity, cigarette smoking, cocaine and other drug use, multiple gestation, chronic hypertension, mild and severe pre-eclampsia, premature rupture of membranes, oligohydramnios, and chorioamnionitis.[23]Oyelese Y, Ananth CV. Placental abruption. Obstet Gynecol. 2006 Oct;108(4):1005-16.
https://www.doi.org/10.1097/01.AOG.0000239439.04364.9a
http://www.ncbi.nlm.nih.gov/pubmed/17012465?tool=bestpractice.com
[24]Tikkanen M, Nuutila M, Hiilesmaa V, et al. Clinical presentation and risk factors of placental abruption. Acta Obstet Gynecol Scand. 2006;85(6):700-5.
https://obgyn.onlinelibrary.wiley.com/doi/10.1080/00016340500449915
http://www.ncbi.nlm.nih.gov/pubmed/16752262?tool=bestpractice.com
Haemolysis, elevated liver enzymes, and low platelet count (HELLP) syndrome
Characterised by haemolytic anaemia, elevated liver enzymes, and thrombocytopenia.
A severe form of pre-eclampsia (sometimes called 'atypical pre-eclampsia’).[25]Erez O, Romero R, Jung E, et al. Preeclampsia and eclampsia: the conceptual evolution of a syndrome. Am J Obstet Gynecol. 2022 Feb;226(2s):S786-803.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8941666
http://www.ncbi.nlm.nih.gov/pubmed/35177220?tool=bestpractice.com
Acute fatty liver of pregnancy
Rare but life-threatening condition characterised by micro-vesicular fatty infiltration of the liver.
Most commonly occurs in the third trimester.[26]Westbrook RH, Dusheiko G, Williamson C. Pregnancy and liver disease. J Hepatol. 2016 Apr;64(4):933-45.
https://www.journal-of-hepatology.eu/article/S0168-8278(15)00788-6/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/26658682?tool=bestpractice.com
Incarceration of the gravid uterus
A rare condition that occurs when the growing uterus becomes entrapped in the pelvis between the pubic symphysis and the sacral promontory, preventing its transition from a pelvic to an abdominal organ.[27]Shnaekel KL, Wendel MP, Rabie NZ, et al. Incarceration of the gravid uterus. Obstet Gynecol Surv. 2016 Oct;71(10):613-9.
http://www.ncbi.nlm.nih.gov/pubmed/27770131?tool=bestpractice.com
If not promptly recognised and treated, incarceration of the gravid uterus is a potentially devastating complication of pregnancy.
Occurrence is estimated to be approximately 1 in 3000 pregnancies.[28]Samejima K, Matsunaga S, Takai Y, et al. Efficacy of well-planned management in patients with incarcerated gravid uterus: a case series and literature review. Taiwan J Obstet Gynecol. 2021 Jul;60(4):679-84.
https://www.sciencedirect.com/science/article/pii/S1028455921001285
http://www.ncbi.nlm.nih.gov/pubmed/34247806?tool=bestpractice.com
Incarceration of the gravid uterus is typically diagnosed in the second trimester (median gestational age of approximately 17 weeks at presentation).[29]Yun F, Fu L, Wen J, et al. Incarceration of the gravid uterus in women with previous cesarean section: case series and literature review. Int J Womens Health. 2025;17:2255-63.
https://pmc.ncbi.nlm.nih.gov/articles/PMC12296648
http://www.ncbi.nlm.nih.gov/pubmed/40718087?tool=bestpractice.com
[30]Ntafam CN, Beutler BD, Harris RD. Incarcerated gravid uterus: a rare but potentially devastating obstetric complication. Radiol Case Rep. 2022 May;17(5):1583-6.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8924533
http://www.ncbi.nlm.nih.gov/pubmed/35309386?tool=bestpractice.com
Gynaecological
Adnexal masses
Incidence of adnexal mass in pregnancy has been reported to be between 0.05% and 6%.[31]Gaughran J, Magee C, Mitchell S, et al. Adnexal masses in pregnancy: a single-centre prospective observational cohort study. diagnostics (Basel). 2024 Sep 30;14(19):2182.
https://pmc.ncbi.nlm.nih.gov/articles/PMC11475458
http://www.ncbi.nlm.nih.gov/pubmed/39410586?tool=bestpractice.com
[32]Cathcart AM, Nezhat FR, Emerson J, et al. Adnexal masses during pregnancy: diagnosis, treatment, and prognosis. Am J Obstet Gynecol. 2023 Jun;228(6):601-12.
https://www.ajog.org/article/S0002-9378(22)02179-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/36410423?tool=bestpractice.com
[33]Cagino K, Li X, Thomas C, et al. Surgical management of adnexal masses in pregnancy: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2021 Jun;28(6):1171-82.e2.
http://www.ncbi.nlm.nih.gov/pubmed/33515746?tool=bestpractice.com
[34]Montes de Oca MK, Dotters-Katz SK, Kuller JA, et al. Adnexal masses in pregnancy. Obstet Gynecol Surv. 2021 Jul;76(7):437-50.
http://www.ncbi.nlm.nih.gov/pubmed/34324696?tool=bestpractice.com
[35]Webb KE, Sakhel K, Chauhan SP, et al. Adnexal mass during pregnancy: a review. Am J Perinatol. 2015 Sep;32(11):1010-6.
http://www.ncbi.nlm.nih.gov/pubmed/26007316?tool=bestpractice.com
Pelvic masses should be considered cancerous until proved otherwise. The vast majority of adnexal cysts in female reproductive-age patients are benign and resolve spontaneously.[32]Cathcart AM, Nezhat FR, Emerson J, et al. Adnexal masses during pregnancy: diagnosis, treatment, and prognosis. Am J Obstet Gynecol. 2023 Jun;228(6):601-12.
https://www.ajog.org/article/S0002-9378(22)02179-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/36410423?tool=bestpractice.com
Consideration of the possibility of malignancy is, however, prudent.
Adnexal torsion, and its recurrence, is more common during pregnancy.[36]Young R, Cork K. Intermittent ovarian torsion in pregnancy. Clin Pract Cases Emerg Med. 2017 May;1(2):108-10.
https://pmc.ncbi.nlm.nih.gov/articles/PMC5965408
http://www.ncbi.nlm.nih.gov/pubmed/29849404?tool=bestpractice.com
[37]Hasson J, Tsafrir Z, Azem F, et al. Comparison of adnexal torsion between pregnant and nonpregnant women. Am J Obstet Gynecol. 2010 Jun;202(6):536.e1-6.
http://www.ncbi.nlm.nih.gov/pubmed/20060090?tool=bestpractice.com
Torsion occurs more frequently on the right side than the left.[36]Young R, Cork K. Intermittent ovarian torsion in pregnancy. Clin Pract Cases Emerg Med. 2017 May;1(2):108-10.
https://pmc.ncbi.nlm.nih.gov/articles/PMC5965408
http://www.ncbi.nlm.nih.gov/pubmed/29849404?tool=bestpractice.com
Exogenous ovarian stimulation (assisted reproductive technology) is a risk factor for adnexal torsion.[37]Hasson J, Tsafrir Z, Azem F, et al. Comparison of adnexal torsion between pregnant and nonpregnant women. Am J Obstet Gynecol. 2010 Jun;202(6):536.e1-6.
http://www.ncbi.nlm.nih.gov/pubmed/20060090?tool=bestpractice.com
[38]Spitzer D, Wirleitner B, Steiner H, et al. Adnexal torsion in pregnancy after assisted reproduction - case study and review of the literature. Geburtshilfe Frauenheilkd. 2012 Aug;72(8):716-20.
https://pmc.ncbi.nlm.nih.gov/articles/PMC4168525
http://www.ncbi.nlm.nih.gov/pubmed/25258463?tool=bestpractice.com
Adnexal mass causing abdominal pain (torsion, haemorrhage, and rupture) is more likely to present in the first trimester.[39]Wang YX, Deng S. Clinical characteristics, treatment and outcomes of adnexal torsion in pregnant women: a retrospective study. BMC Pregnancy Childbirth. 2020 Aug 24;20(1):483.
https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-020-03173-7
http://www.ncbi.nlm.nih.gov/pubmed/32831043?tool=bestpractice.com
[40]Zucchini S, Marra E. Diagnosis of emergencies/urgencies in gynecology and during the first trimester of pregnancy. J Ultrasound. 2014 Mar;17(1):41-6.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3945190
http://www.ncbi.nlm.nih.gov/pubmed/24616750?tool=bestpractice.com
Adnexal masses considered for intervention include those that are:[32]Cathcart AM, Nezhat FR, Emerson J, et al. Adnexal masses during pregnancy: diagnosis, treatment, and prognosis. Am J Obstet Gynecol. 2023 Jun;228(6):601-12.
https://www.ajog.org/article/S0002-9378(22)02179-2/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/36410423?tool=bestpractice.com
[34]Montes de Oca MK, Dotters-Katz SK, Kuller JA, et al. Adnexal masses in pregnancy. Obstet Gynecol Surv. 2021 Jul;76(7):437-50.
http://www.ncbi.nlm.nih.gov/pubmed/34324696?tool=bestpractice.com
persistent, large (>10 cm, present after the first trimester)
at increased risk for torsion
symptomatic
found to have features concerning for malignancy on ultrasound.
Ovarian cyst rupture is rare, and may occur in conjunction with torsion.[41]Barcroft J, Pandrich M, Del Forno S, et al. Evaluating use of two-step International Ovarian Tumor Analysis strategy to classify adnexal masses identified in pregnancy: pilot study. Ultrasound Obstet Gynecol. 2024 Dec;64(6):808-17.
https://pmc.ncbi.nlm.nih.gov/articles/PMC11609963
http://www.ncbi.nlm.nih.gov/pubmed/38787921?tool=bestpractice.com
[42]Asfour V, Varma R, Menon P. Clinical risk factors for ovarian torsion. J Obstet Gynaecol. 2015;35(7):721-5.
https://www.tandfonline.com/doi/10.3109/01443615.2015.1004524
http://www.ncbi.nlm.nih.gov/pubmed/26212687?tool=bestpractice.com
Massive haemorrhage into an ovarian cyst (particularly a malignant cyst) occurs infrequently and causes pain similar to that of torsion.
Haemorrhage may also result in a corpus luteum cyst.[43]Hallatt JG, Steele CH Jr, Snyder M. Ruptured corpus luteum with hemoperitoneum: a study of 173 surgical cases. Am J Obstet Gynecol. 1984 May 1;149(1):5-9.
http://www.ncbi.nlm.nih.gov/pubmed/6720774?tool=bestpractice.com
[44]Cheah G, Liu J. Rare case of haemoperitoneum secondary to a ruptured ovarian ectopic pregnancy superimposed by a bleeding corpus luteum cyst. BMJ Case Rep. 2024 Jan 29;17(1):e256872.
http://www.ncbi.nlm.nih.gov/pubmed/38286579?tool=bestpractice.com
At the time of formation of the corpus luteum, there is always a little bleeding into the follicle that has discharged its ovum. If the bleeding is excessive, the corpus luteum becomes distended with blood. Cysts vary in size from 2.5 to 10 cm.
Fibroids
The incidence of fibroids during pregnancy is unknown; rates of between 0.1% and 12.5% have been reported.[45]Cooper NP, Okolo S. Fibroids in pregnancy: common but poorly understood. Obstet Gynecol Surv. 2005 Feb;60(2):132-8.
http://www.ncbi.nlm.nih.gov/pubmed/15671902?tool=bestpractice.com
[46]Mitro SD, Peddada S, Chen Z, et al. Natural history of fibroids in pregnancy: National Institute of Child Health and Human Development Fetal Growth Studies - singletons cohort. Fertil Steril. 2022 Oct;118(4):656-65.
https://pmc.ncbi.nlm.nih.gov/articles/PMC9529811
http://www.ncbi.nlm.nih.gov/pubmed/35981916?tool=bestpractice.com
Most growth happens in early pregnancy.[47]Ghosh S, Naftalin J, Imrie R, et al. Natural history of uterine fibroids: a radiological perspective. Curr Obstet Gynecol Rep. 2018;7(3):117-21.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6060784
http://www.ncbi.nlm.nih.gov/pubmed/30101039?tool=bestpractice.com
[48]Benaglia L, Cardellicchio L, Filippi F, et al. The rapid growth of fibroids during early pregnancy. PLoS One. 2014;9(1):e85933.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3896432
http://www.ncbi.nlm.nih.gov/pubmed/24465797?tool=bestpractice.com
Cause pain in pregnancy mainly because of red degeneration (necrobiosis), which occurs in 5% to 10% of pregnancies between 12 and 20 weeks' gestation.[45]Cooper NP, Okolo S. Fibroids in pregnancy: common but poorly understood. Obstet Gynecol Surv. 2005 Feb;60(2):132-8.
http://www.ncbi.nlm.nih.gov/pubmed/15671902?tool=bestpractice.com
Pain may also result from torsion of a pedunculated fibroid or from fibroid impaction.[49]Douglas C, Owen A, Muhlmann M. Torted fibroid: a cause of acute abdomen in pregnancy. ANZ J Surg. 2025 Aug 22.
https://onlinelibrary.wiley.com/doi/epdf/10.1111/ans.70304
Urological
Urological conditions in pregnancy present a major diagnostic challenge, as the urinary tract undergoes profound anatomical and physiological changes that predispose pregnant women to an increased risk for symptomatic UTIs and kidney stone formation. The ureters become dilated as early as the first trimester and remain distended until after delivery. This is mainly due to compression exerted by the growing uterus on the collecting system above the level of the linea terminalis. This leads to vascular congestion of the upper urinary tract, with consequent urinary stasis. These changes can facilitate aggregation of crystals in the urine and increase the risk of ascending infection. The following conditions may subsequently occur.
UTI
Most frequently Escherichia coli (80% to 90% of UTIs during pregnancy)
Other gram-negative rods isolated: Proteus mirabilis, Klebsiella pneumonia
Incidence increases with low socio-economic status, increasing age, sexual activity, and diabetes mellitus.
Acute pyelonephritis
Most common during the second half of pregnancy, as a result of increased ureteral obstruction and urinary stasis[50]Sheffield JS, Cunningham FG. Urinary tract infection in women. Obstet Gynecol. 2005 Nov;106(5 Pt 1):1085-92.
http://www.ncbi.nlm.nih.gov/pubmed/16260529?tool=bestpractice.com
Usually uni-lateral and more common in the right kidney
E coli is the predominant organism.
Nephrolithiasis
Usually occurs during the second and third trimesters
Three times more likely in multi-parous women
Ureteric stones more common than kidney stones.[51]Cormier CM, Canzoneri BJ, Lewis DF, et al. Urolithiasis in pregnancy: current diagnosis, treatment, and pregnancy complications. Obstet Gynecol Surv. 2006 Nov;61(11):733-41.
http://www.ncbi.nlm.nih.gov/pubmed/17044950?tool=bestpractice.com
Hydronephrosis
Common physiological condition in pregnancy; disappears rapidly after birth[52]Rasmussen PE, Nielsen FN. Hydronephrosis during pregnancy: a literature survey. Eur J Obstet Gynecol Reprod Biol. 1988 Mar;27(3):249-59.
http://www.ncbi.nlm.nih.gov/pubmed/3280355?tool=bestpractice.com
Most commonly (90%) occurs after the 20th week of gestation, being more pronounced in primigravidae
Dilatation only seen above the linea terminalis and is more frequently right sided
Compression of the ureters by the uterus (causing hydronephrosis) can result in acute attacks of pain triggered by ureteral obstruction.
Gastrointestinal
A number of common gastrointestinal (GI) conditions can complicate pregnancy and present with abdominal pain. In turn, pregnancy can make the diagnosis of these conditions difficult due to the physiological changes occurring to the body during this time.
Appendicitis
Acute appendicitis occurs approximately at a rate of 1:1250 to 1:1500.[53]Kave M, Parooie F, Salarzaei M. Pregnancy and appendicitis: a systematic review and meta-analysis on the clinical use of MRI in diagnosis of appendicitis in pregnant women. World J Emerg Surg. 2019;14:37.
https://www.doi.org/10.1186/s13017-019-0254-1
http://www.ncbi.nlm.nih.gov/pubmed/31367227?tool=bestpractice.com
No single symptom, sign, or laboratory finding is diagnostic for acute appendicitis.[54]Humes DJ, Simpson J. Acute appendicitis. BMJ. 2006 Sep 9;333(7567):530-4.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1562475
http://www.ncbi.nlm.nih.gov/pubmed/16960208?tool=bestpractice.com
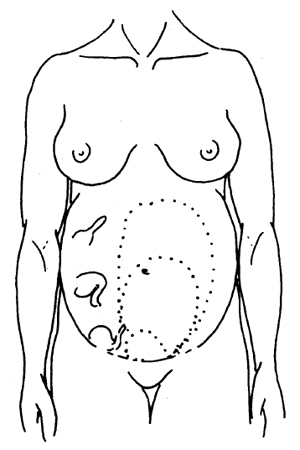
Diagnosis complicated by anatomical changes in the location of the appendix as pregnancy progresses.[55]Pastore PA, Loomis DM, Sauret J, et al. Appendicitis in pregnancy. J Am Board Fam Med. 2006 Nov-Dec;19(6):621-6.
https://www.jabfm.org/content/19/6/621.full
http://www.ncbi.nlm.nih.gov/pubmed/17090795?tool=bestpractice.com
Clinical judgement vital in deciding whether surgical management is needed.[Figure caption and citation for the preceding image starts]: The site of the appendix changes as pregnancy advancesChamberlain G. ABC of antenatal care: abdominal pain in pregnancy. BMJ. 1991;302:390-1394. Used with permission [Citation ends].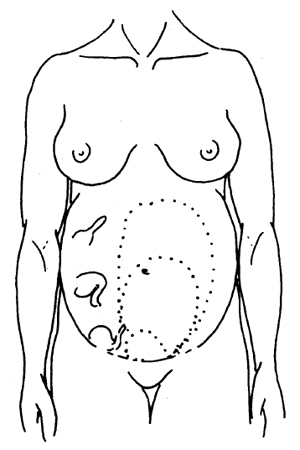
Cholecystitis
Caused by cholelithiasis in >90% of cases in pregnancy.[56]Parangi S, Levine D, Henry A, et al. Surgical gastrointestinal disorders during pregnancy. Am J Surg. 2007 Feb;193(2):223-32.
http://www.ncbi.nlm.nih.gov/pubmed/17236852?tool=bestpractice.com
Cholelithiasis risk is increased by progesterone-induced smooth muscle relaxation of the gallbladder (which promotes stasis of the bile) and elevated levels of oestrogens (which increase the lithogenicity of bile).
Pancreatitis
Cholelithiasis and hypertriglyceridaemia may be common causes in pregnancy.[57]Karsenti D, Bacq Y, Brechot JF, et al. Serum amylase and lipase activities in normal pregnancy: a prospective case-control study. Am J Gastroenterol. 2001 Mar;96(3):697-9.
http://www.ncbi.nlm.nih.gov/pubmed/11280536?tool=bestpractice.com
[58]Tenner S, Vege SS, Sheth SG, et al. American College of Gastroenterology guidelines: management of acute pancreatitis. Am J Gastroenterol. 2024 Mar 1;119(3):419-37.
https://journals.lww.com/ajg/fulltext/2024/03000 american_college_of_gastroenterology_guidelines_.14.aspx
http://www.ncbi.nlm.nih.gov/pubmed/38857482?tool=bestpractice.com
[59]Yang AL, McNabb-Baltar J. Hypertriglyceridemia and acute pancreatitis. Pancreatology. 2020 Jul;20(5):795-800.
http://www.ncbi.nlm.nih.gov/pubmed/32571534?tool=bestpractice.com
Tends to occur late in the third trimester, possibly due to increased intra-abdominal pressure on the biliary ducts.[60]Tang SJ, Rodriguez-Frias E, Singh S, et al. Acute pancreatitis during pregnancy. Clin Gastroenterol Hepatol. 2010 Jan;8(1):85-90.
https://www.cghjournal.org/article/S1542-3565(09)00881-7/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/19747985?tool=bestpractice.com
Intestinal obstruction
Incidence increasing with increased frequency of intra-abdominal surgery, pelvic surgery, and PID.
Most commonly caused by simple obstruction, mainly as a result of adhesions (60% to 70% of cases) or volvulus (25%).[2]Augustin G, Majerovic M. Non-obstetrical acute abdomen during pregnancy. Eur J Obstet Gynecol Rep Biol. 2007 Mar;131(1):4-12.
http://www.ncbi.nlm.nih.gov/pubmed/16982130?tool=bestpractice.com
Rarely caused by intussusception, hernias, and neoplasms.
Traumatic
Traumatic causes of abdominal pain should not be overlooked in pregnant women. Abdominal pain following blunt trauma affects 6% to 7% of pregnancies, 0.3% of which require admission.[61]Shah KH, Simons RK, Holbrook T, et al. Trauma in pregnancy: maternal and fetal outcome. J Trauma. 1998 Jul;45(1):83-6.
http://www.ncbi.nlm.nih.gov/pubmed/9680017?tool=bestpractice.com
The most common causes are road traffic accidents, accidental falls, and physical abuse. Splenic rupture may be due to domestic violence.[62]Bljajic D, Ivanisevic M, Djelmis J, et al. Splenic rupture in pregnancy: traumatic or spontaneous event? Eur J Obstet Gynecol Reprod Biol. 2004 Jul 15;115(1):113-4.
http://www.ncbi.nlm.nih.gov/pubmed/15223180?tool=bestpractice.com
Musculoskeletal
Although uncommon, a rectus sheath haematoma can be the cause of abdominal pain in pregnancy. Trauma, obesity, straining, coughing, previous abdominal surgery, vascular pathologies, disorders of coagulation, endometriosis of the rectus sheath, Cushing's syndrome, and anticoagulation therapy may contribute to the occurrence of this condition.[63]Deb S, Hoo P, Chilaka V. Rectus sheath haematoma in pregnancy: a clinical challenge. J Obstet Gynaecol. 2006 Nov;26(8):822-3.
http://www.ncbi.nlm.nih.gov/pubmed/17130051?tool=bestpractice.com