Aetiology
Aetiology varies with the type of retinal detachment (RD). The condition of the vitreous is extremely important for the development of rhegmatogenous RD. Syneresis, where the normal gel structure gives way to a mixture of gel and fluid, allows the available unbound water to access the sub-retinal space through a retinal break, leading to RD.[12]
Several factors can contribute to structural changes of the vitreous gel. These include:
Age
Myopia
Trauma
Cataract surgery
Ocular inflammation.
Exudative RD may result after inflammation in the vitreous, retina, uvea, or posterior sclera (e.g., Vogt-Koyanagi-Harada syndrome).[2] Other causes include vascular anomalies (e.g., Coats' disease), anatomic anomalies (e.g., optic nerve pit), surgical intervention (e.g., scleral buckling, heavy cryopexy or laser retinopexy), choroidal melanoma, and central serous chorioretinopathy.[2][3][4] The sub-retinal fluid is usually more viscous (higher protein concentration) than in other types of RD.
Haemorrhagic RD results from bleeding into the sub-retinal space. Most cases result from trauma, although age-related macular degeneration causes a significant number. Other relevant systemic conditions include blood dyscrasias and subdural or subarachnoidal bleeding.
Tractional RD usually occurs due to diabetes, retinal vein occlusion, trauma, or previous surgery. In diabetic eyes, proliferative membranes form via a complex process involving capillary non-perfusion and the body's reparative process. In post-traumatic and post-surgical detachments, inflammation and scarring develop in response to normal healing responses.
Pathophysiology
Rhegmatogenous RD develops in response to vitreoretinal traction. For example, posterior vitreous detachment (PVD) may lead to one or more retina breaks. Fluid can then pass from the vitreous cavity into the sub-retinal space, which extends the RD once the amount of incoming fluid exceeds the removal capacity of the retinal pigment epithelium (RPE). Although PVD is a major factor in the pathogenesis of rhegmatogenous RD, no preoperative diagnostic technique can accurately distinguish this from a posterior vitreoschisis. RD progresses based on many factors, including:
Location of the break: superior faster than inferior
Size of the break: larger faster than smaller
Adhesion of the remaining vitreous gel to the retina: stronger faster than weaker
Movement of the patient's head and eyes: lack of such movement (e.g., with bilateral patching) can lead to spontaneous, albeit temporary, reattachment of the retina.
In tractional RD, the membranes on the retinal surface are attached to the retina and contractile. As the membranes contract, the retina detaches from the RPE. Sub-retinal fluid accumulation develops secondarily as part of the normal fluid transport from the vitreous to the choroid and simply fills the space created by the elevated retina.
In serous and haemorrhagic RD, the fluid that accumulates under the neuroretina separates it from the RPE.
Classification
Clinical classification
No internationally described or accepted formal classification exists for RD. Clinicians distinguish sub-types by clinical appearance, pathogenesis, and treatment/prognosis implication.
Rhegmatogenous RD
The direct cause is a retinal break, although traction typically leads to the break forming. The sub-retinal fluid originates in the vitreous. [Figure caption and citation for the preceding image starts]: Retinal detachment approaching the macula, showing typical, full-thickness foldsFrom the collection of Dr F. Kuhn and Dr R. Morris, with permission [Citation ends].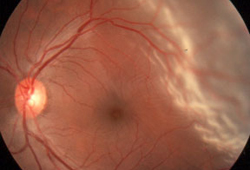
Tractional RD
The cause is a visible and marked vitreoretinal or, rarely, sub-retinal traction that typically originates in the vitreous cavity. Retinal shortening (intraretinal traction) may also develop. The most severe form develops as part of a more widespread scarring process (e.g., PVR). Retinal discontinuity is absent. The sub-retinal fluid originates in the vitreous.[Figure caption and citation for the preceding image starts]: Tractional retinal detachment in a patient with diabetesFrom the collection of Dr F. Kuhn and Dr R. Morris, with permission [Citation ends].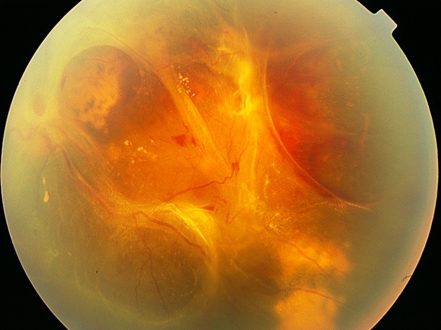
Combined rhegmatogenous/tractional RD
Primarily results from vitreoretinal traction that causes one or more retinal breaks.
Exudative RD
This results from sub-retinal fluid accumulation. It can develop secondary to an inflammatory process in the vitreous, retina, uvea, or posterior sclera (e.g., Vogt-Koyanagi-Harada syndrome).[2] Other causes include vascular anomalies (e.g., Coats disease), surgical intervention (scleral buckling, heavy cryopexy or laser retinopexy), choroidal melanoma, and central serous chorioretinopathy.[2][3][4] The sub-retinal fluid is usually more viscous than in other types of RD. The sub-retinal fluid originates in the retina, choroid, or cerebrospinal space.[Figure caption and citation for the preceding image starts]: Uveitis-related serous retinal detachmentFrom the collection of Dr F. Kuhn and Dr R. Morris, with permission [Citation ends].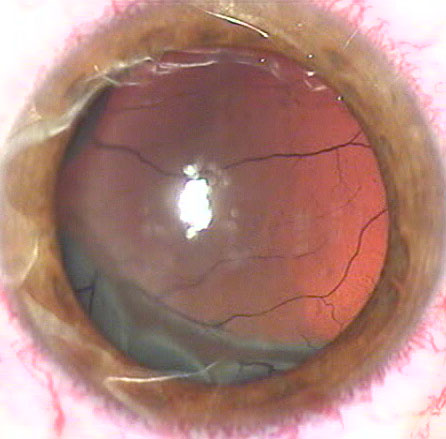
Haemorrhagic RD
Caused by bleeding into the sub-retinal space.
Use of this content is subject to our disclaimer