Investigations
1st investigations to order
stool examination
Test
Microscopic identification of eggs and proglottids in the stool is diagnostic for taeniasis. However, it may take 2-3 months for these to appear in the faeces of the host once the adult tapeworm is established.[3] Egg release in the stool may be variable because of irregular rates of proglottid detachment and degeneration.
Examination of the stool samples over several days increases the yield. Three separate stool samples taken on different days is recommended in order to increase sensitivity.[3]
Species identification is important, and is usually based on morphology of the proglottids. The eggs of Taenia species cannot be distinguished; therefore, it is necessary to obtain mature gravid proglottids, which can differentiate between the tapeworms.[3]
Identification of Taenia solium is significant, and should prompt consideration of possible cysticercosis in index patients or among household contacts.
Diphyllobothrium latum and Hymenolepis nana may be diagnosed by finding characteristic ova in the faeces.
Result
eggs and (gravid/non-gravid) proglottids in stool
full blood count
Test
Should be ordered in all patients to detect eosinophilia caused by parasitic migration through host tissue. Many patients with Hymenolepis nana have moderate eosinophilia.
Diphyllobothrium latum infections may present with megaloblastic pernicious anaemia due to absorption of vitamin B12 by the tapeworm.
About 40% of people harbouring the worm have reduced serum vitamin B12, but fewer than 2% develop anaemia.[49]
Result
moderate eosinophilia, megaloblastic pernicious anaemia
enzyme-linked immunoelectrotransfer blot (EITB)
Test
Serologic testing is usually required for the diagnosis of cysticercosis, particularly if other diagnostic criteria are not met (e.g., cystic lesion confirmed on imaging).[44] Recommended as a confirmatory test in patients with neurocysticercosis.[43][44]
EITB is an immunoblot using seven purified glycoprotein antigens. It has 98% sensitivity and 100% specificity in patients with more than one lesion.
Sensitivity in single-cyst cases may drop to 70%.[45]
Result
Taenia solium with purified glycoprotein antigens (Western blot)
echinococcus enzyme-linked immunosorbent assay (ELISA) and Western blot serology
Test
Serological testing may be used for the diagnosis of echinococcosis when imaging is not conclusive.[20]
Western blot is the confirmatory test for Echinococcus. Serology is 80% to 100% sensitive and 88% to 96% specific for liver cyst infections.
It is less sensitive for lung involvement (50%-56%) and 25% to 26% for other organ involvement.[1]
In the US, ELISA is available through the Centers for Disease Control and Prevention (CDC).
Result
Echinococcus species with purified glycoprotein antigens (Western blot)
abdominal/thoracic ultrasound
Test
Abdominal or thoracic ultrasound may detect hydatid cysts (e.g., echinococcosis of the liver or lungs).
The World Health Organization (WHO) classifies the stages of Echinococcus granulosus into active versus inactive, and classification guides therapy.[20] See Criteria.
[Figure caption and citation for the preceding image starts]: Echinococcus of liver with daughter cyst on ultrasound: multivesicular, multiseptated cysts, where daughter cyst completely fills the unilocular mother cyst; cyst produces a wheel-like structureFrom the personal collections of Dr Christina Coyle and Dr Maheen Saeed; used with permission [Citation ends].
Result
hydatid cysts
MRI of chest/abdomen
echocardiogram
Test
Echocardiography is typically used to diagnose cardiac cystic echinococcosis, alongside other imaging modalities.[38]
Result
hydatid cysts
CT of brain
Test
Neuroimaging is the mainstay of diagnosis for neurocysticercosis.[43][44][47] MRI is superior to CT in identifying extraparenchymal cysts and posterior fossa lesions, but CT is better in visualising calcified cysts.[46] Ideally, both tests should be considered.
Specific findings depend on the location of the cysts.
Cysts may be parenchymal (non-viable calcified): nodular calcifications <20 mm in diameter (often 1-5 mm) with or without surrounding oedema and/or contrast enhancement.[43]
Cysts may be parenchymal (viable): vesicular lesion with evidence of contrast enhancement and/or surrounding oedema; scolex is often visible.
Cysts may be parenchymal (single small enhancing): cystic or nodular enhancing lesion <2 cm.[43]
Cysts may be extraparenchymal (intraventricular): cysticerci within ventricles; obstructive or loculated hydrocephalus with disproportionate dilation of ventricles.[43]
Cysts may be extraparenchymal (subarachnoid): cysticerci in Sylvian fissure, basilar cisterns, or interhemispheric spaces.[43]
Cysts may be extraparenchymal (spinal): cysticerci in spinal subarachnoid space with or without inflammation/diffuse spinal arachnoiditis; intramedullary cysticerci within spinal cord.[43][Figure caption and citation for the preceding image starts]: Colloidal stage - neurocysticercosis: CT scan showing ring enhancing cystic lesion in the temporal lobe and perilesional oedemaFrom the personal collections of Dr Christina Coyle and Dr Maheen Saeed; used with permission [Citation ends].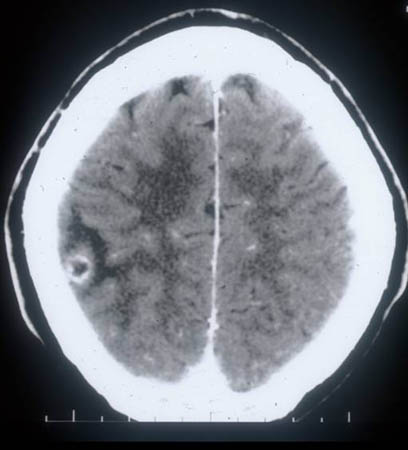
Result
brain calcifications are common; specific findings depend on the location of the cysts
MRI of brain/spine
Test
Neuroimaging is the mainstay of diagnosis for neurocysticercosis.[43][44][47] MRI is superior to CT in identifying extraparenchymal cysts and posterior fossa lesions, but CT is better in visualising calcified cysts.[46] MRI may also reveal the scolex, which is usually not visible on CT scans. Ideally, both tests should be considered.
Specific findings depend on the location of the cysts (see CT of brain, above).[43][47]
All patients with subarachnoid disease should also have an MRI of the spine.[43][Figure caption and citation for the preceding image starts]: Cystic stage - neurocysticercosis: MRI scan showing cystic lesion in the frontal lobe; a scolex can be seen within the cystFrom the personal collections of Dr Christina Coyle and Dr Maheen Saeed; used with permission [Citation ends]. [Figure caption and citation for the preceding image starts]: Granular stage - neurocysticercosis: MRI scan showing enhancing lesion without perilesional oedemaFrom the personal collections of Dr Christina Coyle and Dr Maheen Saeed; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Granular stage - neurocysticercosis: MRI scan showing enhancing lesion without perilesional oedemaFrom the personal collections of Dr Christina Coyle and Dr Maheen Saeed; used with permission [Citation ends].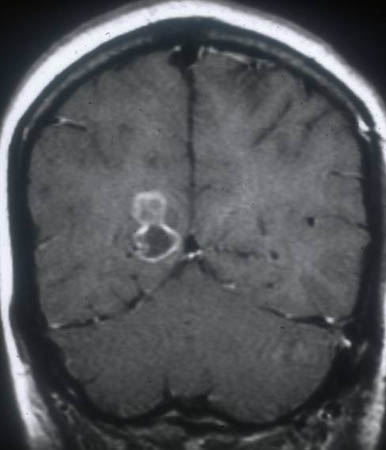 [Figure caption and citation for the preceding image starts]: Calcified stage - neurocysticercosis: MRI scan of multiple calcified lesions in a patient with neurocysticercosisFrom the personal collections of Dr Christina Coyle and Dr Maheen Saeed; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Calcified stage - neurocysticercosis: MRI scan of multiple calcified lesions in a patient with neurocysticercosisFrom the personal collections of Dr Christina Coyle and Dr Maheen Saeed; used with permission [Citation ends].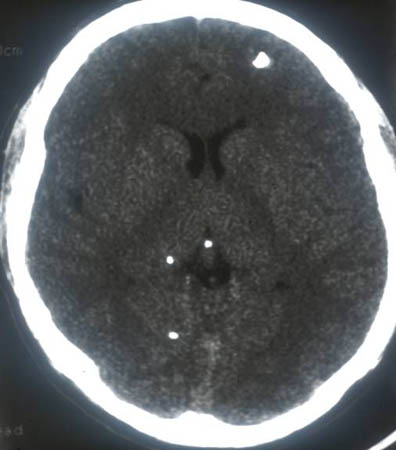
Result
extraparenchymal cysticerci tapeworm scolex; specific findings depend on the location of the cysts
Investigations to consider
screening for tuberculosis and strongyloidiasis
Test
Screening for latent tuberculosis and strongyloidiasis is recommended in patients who are likely to require long-term corticosteroid therapy (i.e., 1 month or more) for neurocysticercosis, due to the risk of immunosuppression and opportunistic infections with this type of treatment.[43]
Result
Strongyloides larvae seen on stool examination (strongyloidiasis); positive interferon-gamma release assay or positive tuberculin skin test (tuberculosis)
Use of this content is subject to our disclaimer