Investigations
1st investigations to order
binocular red reflex test (Brückner test)
Test
A direct ophthalmoscope examination should show a symmetric and bright yellow or red reflex in each normal pupil.
The test can detect media opacities (diminished reflex or opacity within the reflex), strabismus (diminished reflex or absent reflex in the eye not directed towards the direct ophthalmoscope light), or high refractive error. An absent or irregular red reflex, or opacity within the reflex, can indicate visual axis obstruction (e.g., due to cataract or intra-ocular tumour).
Red reflex testing should be undertaken before applying cycloplegic agents for pupillary dilation.
Result
may show media opacities, strabismus, or high refractive error
visual acuity tests (monocular)
Test
Verbal children are best tested with multiple rather than single optotypes.[40]
Although amblyopic eyes see better when a single optotype is presented on a blank background, which can lead to overestimated visual acuity, some young children may get distracted or confused when presented with multiple optotypes. Crowding bars (i.e., stripes that surround an individual target to simulate multiple targets) may be used to avoid overestimating visual acuity. Subjective visual acuity testing is preferred if children can participate reliably, but instrument-based screening (e.g., photoscreening or autorefraction) may be useful in children who are unable to cooperate with testing.
Result
reduced, and does not normalise with correction of refractive error alone
stereopsis/binocular vision testing
Test
Sensorimotor fusion and coordinated binocular eye movements are sensitive to disruption by amblyopia.[1][42][43]
Stereopsis (the perception of 3-dimensionality, or depth) is an important component of binocular vision testing, typically assessed using random dot-based global tests. The Randot Circles test presents contoured circles at 10 discrete disparity levels from 20 to 400 arcs and tasks the patient to choose which of 3 circles at each disparity level appears closest (a simple forced choice, with a lower arc second number indicating better stereopsis). Several other tests are also available depending on local practice and clinical need (e.g., TNO, Lang, Titmus, and Frisby).
Additional testing for stereoacuity may include evaluation of sensory fusion (e.g., The Worth 4-Dot Test) and fusional motor vergence (e.g., prism bar or rotary prism testing).
Degree of stereopsis is reported as the number of arc seconds, with lower numbers (40 arc seconds) indicating better stereopsis than higher numbers (3000 arc seconds).
Result
frequently reduced
assessment of fixation, ocular alignment, and ocular motility
Test
Patients with a clear visual axis to the fovea and with a normally positioned fovea fixate with the centre of the eye, whereas patients with amblyopia, visual axis opacity, or displacement or disease involving the fovea may fixate eccentrically, as if looking at an object from the side.
Marked eccentric fixation is detected by observing the non-central position of the corneal reflection in the amblyopic eye while the amblyopic eye fixates on a light.
A patient with strabismus who can freely alternate fixation between the eyes does not have amblyopia.
Fixation can be graded according to whether the non-preferred eye holds fixation momentarily, for a few seconds (or to or through a blink), or does not hold fixation, or whether there is spontaneous alternation of fixation.[1]
Cover testing is used in the assessment of tropias and total deviation in primary gaze.[1]
During assessment, the ophthalmologist pays special attention to anomalous head postures and ocular motility that may suggest refractive error, strabismus, or nystagmus.
Ocular alignment testing should be undertaken before cycloplegia to avoid any temporary induced shifts in alignment.
Result
fixation may be central or eccentric; ocular alignment tests may reveal strabismus; ocular motility may be abnormal
anterior segment examination using a slit lamp
Test
Helps exclude ocular pathologies that contribute to decreased vision (e.g., cataracts).
Although these defects may be solely responsible for vision loss, co-existent amblyopia may explain a portion of the vision loss if they occur asymmetrically or monocularly.[Figure caption and citation for the preceding image starts]: Slit lampFrom the collection of Tina Rutar, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Author performing slit lamp examFrom the collection of Tina Rutar, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Author performing slit lamp examFrom the collection of Tina Rutar, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Portable slit lampFrom the collection of Tina Rutar, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Portable slit lampFrom the collection of Tina Rutar, MD [Citation ends].
Performed with a slit lamp; young children may require a portable slit lamp or magnifier.
Result
may reveal ocular pathologies contributing to decreased vision (e.g., cataract)
dilated fundoscopy
Test
Helps exclude ocular pathologies that may contribute to decreased vision (e.g., macular lesions). Although these defects may be solely responsible for vision loss, co-existent amblyopia may explain a portion of the vision loss if they occur asymmetrically or monocularly.[Figure caption and citation for the preceding image starts]: Indirect ophthalmoscope with 28-dioptre lens for performing fundus examinationFrom the collection of Tina Rutar, MD [Citation ends]. [Figure caption and citation for the preceding image starts]: Author performing indirect ophthalmoscopyFrom the collection of Tina Rutar, MD [Citation ends].
[Figure caption and citation for the preceding image starts]: Author performing indirect ophthalmoscopyFrom the collection of Tina Rutar, MD [Citation ends].
Fundoscopic examination is preferably undertaken using an indirect ophthalmoscope and condensing lens. Typically performed after cycloplegic retinoscopy when there is adequate pupillary dilation.[1]
Result
may reveal ocular pathologies contributing to decreased vision (e.g., macular lesions)
cycloplegic retinoscopy
Test
Many causes of amblyopia can only be assessed with a reliable cycloplegic retinoscopy.
Eye drops are used to dilate the pupil and relax the ciliary muscle: cyclopentolate 0.2%/phenylephrine 1% for infants and cyclopentolate 1% (occasionally with phenylephrine 2.5%) for toddlers (children aged 1-3 years) and older children.
A relaxed ciliary muscle impairs the strong focusing ability of the child's eye, allowing the ophthalmologist to objectively determine the child's refractive state.
While performing retinoscopy, the ophthalmologist also assesses the quality of the light reflex to ensure that nothing in the visual axis interferes with a clear image reaching the retina.[Figure caption and citation for the preceding image starts]: Retinoscope with plus and minus spherical lenses for refractionFrom the collection of Tina Rutar, MD [Citation ends].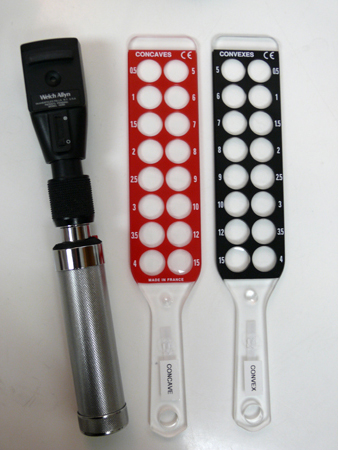
Result
abnormal refractive state, dull retinoscopic reflex, or partially opacified retinoscopic reflex may be present
Emerging tests
visual evoked potentials (VEPs)
Test
May be used to aid diagnosis in uncertain cases.[44][45][46][47][48]
Patterns are recorded using occipital electrodes that detect activity in the visual cortex while visual stimuli are presented to the eyes. Studies using different types of VEPs (orientation-specific, steady-state motion, multifocal, pattern, and sweep) show that these may be used to predict response to amblyopia therapy.[45][46][47][48]
Result
still to be clearly defined
Use of this content is subject to our disclaimer