Investigations
1st investigations to order
gastroscopy
Test
Refer all patients with suspected acute upper gastrointestinal (GI) bleeding for upper GI endoscopy (i.e., gastroscopy).[34][35][36] Follow your local protocol for recommendations on the optimal timing of the procedure for your patient. Guidelines from the National Institute for Health and Care Excellence (NICE) in the UK and the European Society of Gastrointestinal Endoscopy (ESGE), and a consensus care bundle led by the British Society of Gastroenterology (BSG), agree that endoscopy should always be performed within 24 hours of presentation with suspected acute upper GI bleed. However, the exact timing of the procedure within the 24-hour period is controversial and specific recommendations from NICE, the BSG, and the ESGE differ as follows.
The ESGE recommends upper GI endoscopy ≤24 hours from presentation following haemodynamic resuscitation. The ESGE does not recommend urgent (defined by the ESGE as ≤12 hours from presentation) endoscopy.[35]
NICE and the BSG care bundle recommend:[34][36]
Urgent endoscopy, immediately after resuscitation, if the patient is unstable with severe acute upper GI bleeding
Endoscopy within 24 hours of admission for all other patients with upper GI bleeding.
In the absence of data on urgent endoscopy for unstable and high-risk patients, the NICE guideline development group (GDG) based their recommendation for urgent endoscopy on consensus expert opinion of the GDG.[36] The BSG consensus care bundle acknowledges that endoscopy performed <12 hours after presentation in patients with acute non-variceal upper GI bleeding is controversial, and notes that several studies associate endoscopy performed <12 hours after presentation with adverse outcomes.[34][41][42][43][44] The ESGE also recognises that the evidence in the area is conflicting; the ESGE bases their recommendation on studies showing that urgent (defined by the ESGE as ≤12 hours from presentation) endoscopy is associated with worse patient outcomes or with no improvement in clinical outcomes compared with non-urgent early endoscopy.[43][45][46]
[Figure caption and citation for the preceding image starts]: Actively bleeding tear appears as a red longitudinal defect with normal surrounding mucosaFrom the collection of Juan Carlos Munoz, MD, University of Florida [Citation ends].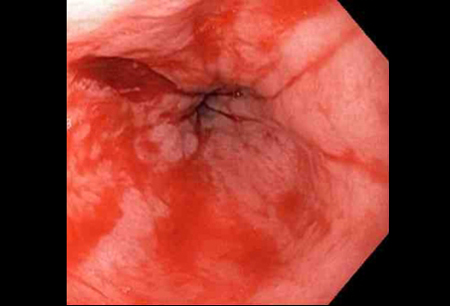
From the personal collection of Douglas Adler; used with permission
Practical tip
Before diagnostic endoscopy consider intubating the patient if needed (e.g., if there is haematemesis, or there is a perceived risk of a haemodynamically unstable patient having blood in the stomach, or if the patient presents with an altered mental status). Make sure the patient is appropriately resuscitated before undergoing diagnostic endoscopy.
Gastroscopy is the test of choice for diagnosis and treatment.[35][36]
An MWT is usually seen at or below the gastro-oesophageal junction as a single linear defect, with normal surrounding mucosa.
An MWT typically varies in length from a few millimetres to several centimetres.
Co-existing lesions are common and may contribute to the bleeding process (e.g., peptic ulcer, erosive oesophagitis).
Practical tip
The tear is often, but not always, seen between 2 o’ clock and 6 o'clock at or below the gastro-oesophageal junction.
Result
tear or laceration typically appears as a red longitudinal defect with normal surrounding mucosa; the lesions vary from a few millimetres to several centimetres
full blood count
Test
Should be part of the initial blood work in any patient with haemorrhage to evaluate the severity of the bleeding and to monitor patients.
The British Society of Gastroenterology consensus care bundle recommends following a restrictive transfusion protocol (trigger: Hb <70 g/L; target: 70–100 g/L) in haemodynamically stable patients. Consider a higher trigger for transfusion than Hb <70 g/L in patients with ischaemic heart disease or haemodynamic instability.[34]
Result
Hb, haematocrit, and platelets are usually unremarkable in an acute setting; however, anaemia may range from mild to severe in rare cases
urea and creatinine
Test
Should be part of the initial evaluation in any patient who presents with haemorrhage.
Urea/creatinine ratio is an important parameter to evaluate the severity of bleeding and to monitor the patient. Urea level at initial presentation is considered a weak predictor of the severity of upper gastrointestinal bleeding.[48]
Result
elevated urea in patients with ongoing bleeding
liver function tests
Test
Should be part of the initial blood work in any patient with haemorrhage.
Used to rule out liver disease, which may predispose a patient to oesophageal varices, gastric varices, or portal hypertensive gastropathy as potential sources of bleeding.
Result
typically normal, except in a patient with underlying or co-existing liver disease
cross-matching/blood grouping
Test
Should be part of the initial blood work in any patient with haemorrhage.
Send blood for typing and cross-matching.
Patients with upper gastrointestinal bleeding can experience rapid clinical deterioration. Blood products may become necessary.
Candidates for blood transfusion include patients with anaemia at presentation or those with ongoing bleeding.
Result
variable
Investigations to consider
prothrombin time/international normalised ratio (PT/INR)
Test
Order in all patients on anticoagulants or in those suspected of coagulopathy.
Prolonged PT times may be a result of anticoagulation therapy, liver pathology, lupus, and other coagulopathies.
Result
typically normal except in a patient with underlying or co-existing liver disease or on anticoagulants
activated partial thromboplastin time (PTT)
Test
Order in all patients on anticoagulants or in those suspected of coagulopathy.
Prolonged PTT times may be a result of anticoagulation therapy, liver pathology, lupus, and other coagulopathies.
Result
typically normal
chest and abdominal CT
Test
Consider chest and abdominal CT scans first line in patients with perforation, suspected peritonitis or a deep tissue injury caused by an MWT.[47] These patients will have significant chest pain, dysphagia, or respiratory symptoms. Laceration or tear without transmural perforation is likely not visible on CT.
Result
typically normal in uncomplicated MWT; may show oesophageal intramural haematoma associated with deep tissue injury, perforation, peritonitis, the source of the bleed
chest x-ray
Test
Consider a chest x-ray in patients suspected of having a complication such as an oesophageal perforation if CT scanning is not available.[32]
Laceration or tear is not visible under conventional radiography.
Result
typically normal in uncomplicated MWT, subcutaneous emphysema may be visible associated with oesophageal rupture
CT angiogram
Test
Consider a CT angiogram in patients with refractory bleeding requiring arterial embolisation. Use the CT angiogram to localise the bleeding site and define the arterial anatomy.[47]
Result
location of bleeding, arterial anatomy
Use of this content is subject to our disclaimer
