Summary
Definition
History and exam
Other diagnostic factors
- light-headedness/dizziness
- postural/orthostatic hypotension
- dysphagia or odynophagia
- retrosternal, epigastric, or back pain
- melaena
- haematochezia
- shock
- signs of anaemia
Risk factors
- condition predisposing to retching, vomiting, and/or straining
- chronic cough
- hiatal hernia
- endoscopy or other instrumentation
- heavy alcohol use
- age 30 to 50 years
- male sex
- hiccups
- blunt abdominal trauma
- cardiopulmonary resuscitation
Diagnostic investigations
1st investigations to order
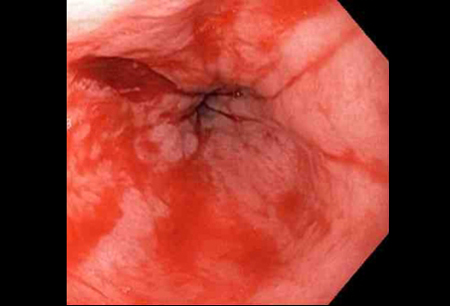
- gastroscopy
- full blood count
- urea and creatinine
- liver function tests
- cross-matching/blood grouping
Investigations to consider
- prothrombin time/international normalised ratio (PT/INR)
- activated partial thromboplastin time (PTT)
- chest and abdominal CT
- chest x-ray
- CT angiogram
Treatment algorithm
Contributors
Expert advisers
Ian Beales, BSc, FEBG, MD, MRCP
Consultant Gastroenterologist
Department of Gastroenterology
Norfolk and Norwich University Hospital
Norwich
UK
Disclosures
IB declares that he has no competing interests.
Acknowledgements
BMJ Best Practice would like to gratefully acknowledge the previous expert contributor, whose work is retained in parts of the content:
Neeraj Bhala DPhil(Oxon), FRACP, FRCPE
Consultant Gastroenterologist
Site Lead of Gastrointestinal Medicine
Queen Elizabeth Hospital
University Hospitals Birmingham
Birmingham
UK
Disclosures
NB declares that he has no competing interests.
Peer reviewers
Adrian Stanley, MBChB, MD, FRCPEd, FRCPSGlasg
Honorary Professor
Consultant Gastroenterologist
NHS Greater Glasgow and Clyde
Glasgow
UK
Disclosures
AS declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Siau K, Hearnshaw S, Stanley AJ, et al. British Society of Gastroenterology (BSG)-led multisociety consensus care bundle for the early clinical management of acute upper gastrointestinal bleeding. Frontline Gastroenterol. 2020 Mar 27;11(4):311-23.Full text Abstract
Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) guideline - update 2021. Endoscopy. 2021 Mar;53(3):300-32.Full text Abstract
National Institute for Health and Care Excellence. Acute upper gastrointestinal bleeding in over 16s: management. August 2016 [internet publication].Full text
Reference articles
A full list of sources referenced in this topic is available here.
Use of this content is subject to our disclaimer