Aetiology
MWT can be caused by: coughing, retching, vomiting, straining, hiccups, closed-chest pressure or cardiopulmonary resuscitation, acute abdominal blunt trauma, alcohol, chemotherapeutic agents, and oesophageal instrumentation.
Hiatal hernia is considered by many to be a key precipitating factor.[6][17][18] However, in >40% of patients an identifiable risk factor is not found.[16]
Conditions that may induce vomiting include:[14][19][20][21]
Gastrointestinal disease (e.g., food poisoning [particularly when due to Bacillus cereus, in which case vomiting occurs soon after ingestion of contaminated food], infectious gastroenteritis, peptic ulcer disease, malrotation, intussusception, volvulus, gastric outlet obstruction, and gastroparesis)
Hepatobiliary disease (e.g., hepatitis, gallstones, and cholecystitis)
Hyperemesis gravidarum
Renal disease (e.g., urinary tract infection, nephrolithiasis, renal failure, and ureteropelvic obstruction)
Neurological disease (e.g., tumours, hydrocephalus, congenital disease, trauma, meningitis, intracranial hypertension, migraine headaches, and seizures)
Psychiatric disease (e.g., anorexia nervosa, bulimia, and cyclic vomiting syndrome).
Other conditions or agents that may induce vomiting include:[22][23][24]
Toxins
Chemotherapy agents (e.g., cisplatin)
Post-anaesthesia or post-surgery.
A chronic cough may be associated with whooping cough, bronchitis, bronchiectasis, emphysema, chronic obstructive pulmonary disease, or lung cancer.[25][Figure caption and citation for the preceding image starts]: Bleeding Mallory Weiss Tear viewed on retroflexionFrom the personal collection of Douglas Adler; used with permission [Citation ends].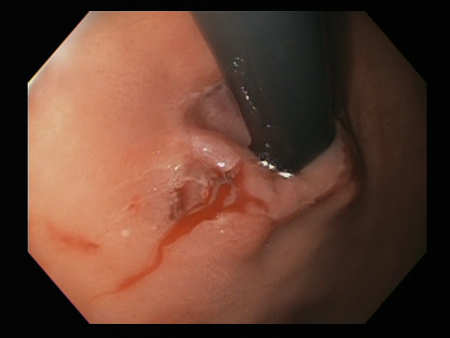
Pathophysiology
The pathogenesis of MWT is not completely understood. Most cases seem to occur as a result of a sudden rise in abdominal pressure or transmural pressure gradient across the gastro-oesophageal junction with a corresponding low intrathoracic pressure. When these forces are high enough to cause distention in this area, an acute gastro-oesophageal tear or laceration may occur.
Classification
Number of lesions
MWT is generally classified by the number of lesions/tears:
Single tear
Multiple tears.
Endoscopic classification[3]
No specific scoring system has been widely adopted or validated for Mallory-Weiss tear (MWT). The Forrest classification, which was specifically designed for bleeding peptic ulcers, has effectively been applied to the prognostication and treatment of bleeding MWT.[4] However, in this context, the classification only considered bleeding stigmata and did not include the impact of complications secondary to deeper tears in the oesophageal mucosa (including intramucosal haemorrhage and transmural perforation) that can be associated with MWT.
For practical purposes, this endoscopic classification based on endoscopic features of the tear remains relevant.
Clean base
Non-bleeding adherent clot
Non-bleeding visible vessel (before or after clot removal)
Actively bleeding or spurting
Oesophageal rupture or perforation (Boerhaave's syndrome).
[Figure caption and citation for the preceding image starts]: Bleeding Mallory Weiss Tear viewed on retroflexionFrom the personal collection of Douglas Adler; used with permission [Citation ends].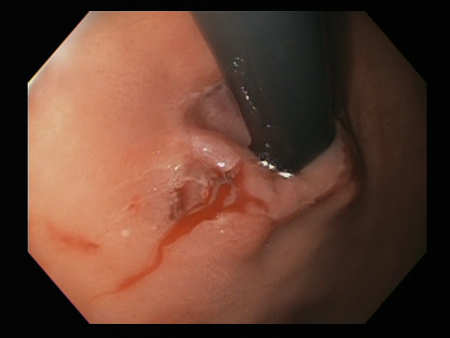 [Figure caption and citation for the preceding image starts]: Mallory Weiss tear after application of through-the-scope clip results in haemostasisFrom the personal collection of Douglas Adler; used with permission [Citation ends].
[Figure caption and citation for the preceding image starts]: Mallory Weiss tear after application of through-the-scope clip results in haemostasisFrom the personal collection of Douglas Adler; used with permission [Citation ends].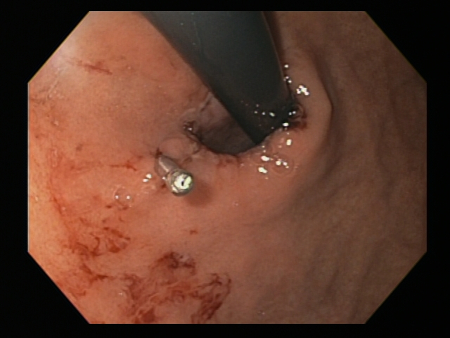
Use of this content is subject to our disclaimer